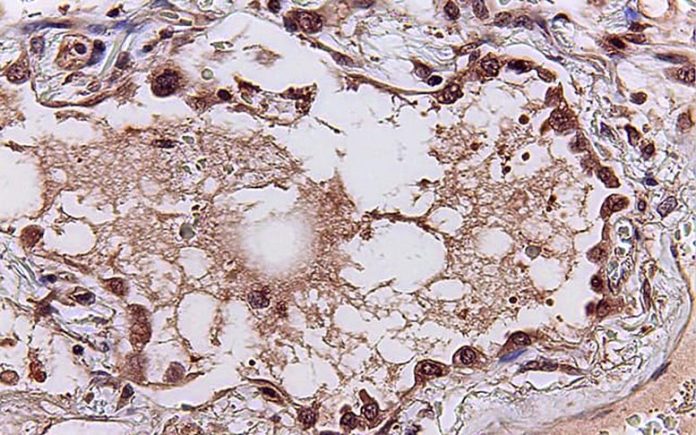
This image reveals specialized lung cells (looking like a beaded pendant) that might install a cytokine storm in action to some viral infections. Credit: UC San Diego Health Sciences
Gene expression patterns related to pandemic viral infections supply a map to assist specify clients’ immune reactions, procedure illness seriousness, forecast results and test treatments — for existing and future pandemics.
Researchers at University of California San Diego School of Medicine utilized an expert system (AI) algorithm to sort through terabytes of gene expression information — which genes are “on” or “off” throughout infection — to search for shared patterns in clients with previous pandemic viral infections, consisting of SARS, MERS and swine influenza.
Two obvious signatures emerged from the research study, released today (June 11, 2021) in eBiomedicine. One, a set of 166 genes, exposes how the human body immune system reacts to viral infections. A 2nd set of 20 signature genes forecasts the seriousness of a client’s illness. For example, the requirement to hospitalize or utilize a mechanical ventilator. The algorithm’s energy was verified utilizing lung tissues gathered at autopsies from departed clients with COVID-19 and animal designs of the infection.
“These viral pandemic-associated signatures tell us how a person’s immune system responds to a viral infection and how severe it might get, and that gives us a map for this and future pandemics,” stated Pradipta Ghosh, MD, teacher of cellular and molecular medication at UC San Diego School of Medicine and Moores Cancer Center.

From a basic blood draw, gene expression patterns related to pandemic viral infections might supply clinicians with a map to assist specify clients’ immune reactions, procedure illness seriousness, forecast results, and test treatments. Credit: UC San Diego Health Sciences
Ghosh co-led the research study with Debashis Sahoo, PhD, assistant teacher of pediatrics at UC San Diego School of Medicine and of computer technology and engineering at Jacobs School of Engineering, and Soumita Das, PhD, associate teacher of pathology at UC San Diego School of Medicine.
During a viral infection, the body immune system launches little proteins called cytokines into the blood. These proteins direct immune cells to the website of infection to assist eliminate the infection. Sometimes, however, the body launches a lot of cytokines, developing a runaway body immune system that assaults its own healthy tissue. This incident, called a cytokine storm, is thought to be among the factors some virally contaminated clients, consisting of some with the typical influenza, catch the infection while others do not.
But the nature, level, and source of deadly cytokine storms, who is at biggest threat, and how it may best be dealt with have actually long been uncertain.
“When the COVID-19 pandemic began, I wanted to use my computer science background to find something that all viral pandemics have in common — some universal truth we could use as a guide as we try to make sense of a novel virus,” Sahoo stated. “This coronavirus may be new to us, but there are only so many ways our bodies can respond to an infection.”
The information utilized to check and train the algorithm originated from openly offered sources of client gene expression information — all the RNA transcribed from clients’ genes and found in tissue or blood samples. Each time a brand-new set of information from clients with COVID-19 appeared, the group checked it in their design. They saw the very same signature gene expression patterns whenever.
“In other words, this was what we call a prospective study, in which participants were enrolled into the study as they developed the disease and we used the gene signatures we found to navigate the uncharted territory of a completely new disease,” Sahoo stated.
By taking a look at the source and function of those genes in the very first signature gene set, the research study likewise exposed the source of cytokine storms: the cells lining lung respiratory tracts and leukocyte called macrophages and T cells. In addition, the outcomes lit up the effects of the storm: damage to those very same lung air passage cells and natural killer cells, a specific immune cell that eliminates virus-infected cells.
“We could see and show the world that the alveolar cells in our lungs that are normally designed to allow gas exchange and oxygenation of our blood, are one of the major sources of the cytokine storm, and hence, serve as the eye of the cytokine storm,” Das stated. “Next, our HUMANOID Center team is modeling human lungs in the context of COVID-19 infection in order to examine both acute and post-COVID-19 effects.”
The scientists believe the details may likewise assist guide treatment techniques for clients experiencing a cytokine storm by supplying cellular targets and criteria to determine enhancement.
To test their theory, the group pre-treated rodents with either a precursor variation of Molnupiravir, a drug presently being checked in scientific trials for the treatment of COVID-19 clients, or SARS-CoV-2-neutralizing antibodies. After direct exposure to SARS-CoV-2, the lung cells of control-treated rodents revealed the pandemic-associated 166- and 20-gene expression signatures. The cured rodents did not, recommending that the treatments worked in blunting cytokine storm.
“It is not a matter of if, but when the next pandemic will emerge,” stated Ghosh, who is likewise director of the Institute for Network Medicine and executive director of the HUMANOID Center of Research Excellence at UC San Diego School of Medicine. “We are building tools that are relevant not just for today’s pandemic, but for the next one around the corner.”
Reference: 11 June 2021, eBiomedicine.
DOI: 10.1016/j.ebiom.2021.103390
Co-authors of the research study consist of: Gajanan D. Katkar, Soni Khandelwal, Mahdi Behroozikhah, Amanraj Claire, Vanessa Castillo, Courtney Tindle, MacKenzie Fuller, Sahar Taheri, Stephen A. Rawlings, Victor Pretorius, David M. Smith, Jason Duran, UC San Diego; Thomas F. Rogers, Scripps Research and UC San Diego; Nathan Beutler, Dennis R. Burton, Scripps Research; Sydney I. Ramirez, La Jolla Institute for Immunology; Laura E. Crotty Alexander, VA San Diego Healthcare System and UC San Diego; Shane Crotty, Jennifer M. Dan, La Jolla Institute for Immunology and UC San Diego.
Funding: National Institutes for Health, UC San Diego Sanford Stem Cell Clinical Center, La Jolla Institute for Immunology Institutional Funds, and VA San Diego Healthcare System