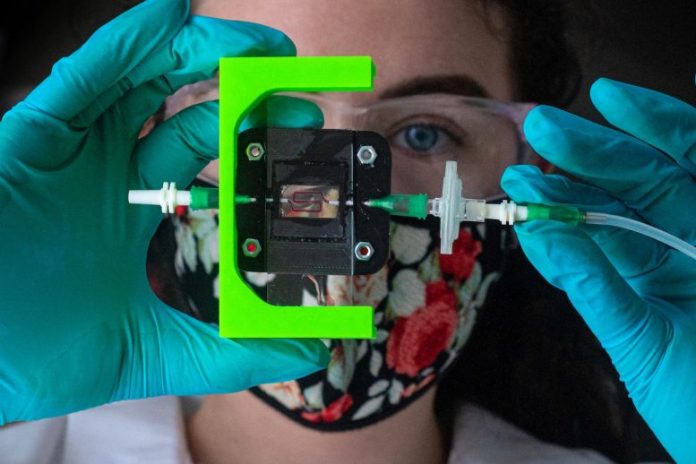
Rice University bioengineers are creating a vascularized, insulin-producing implant for Type 1 diabetes. Graduate trainee Madison Royse shows a lab setup for screening blood circulation through 3D-printed hydrogels that can be developed into living tissue. Credit: Photo by Jeff Fitlow/Rice University
JDRF funds development of implant to immediately control blood sugar levels.
Rice University bioengineers are utilizing 3D printing and wise biomaterials to develop an insulin-producing implant for Type 1 diabetics.
The three-year task is a collaboration in between the labs of Omid Veiseh and Jordan Miller that’s supported by a grant from JDRF, the leading worldwide funder of diabetes research study. Veiseh and Miller will utilize insulin-producing beta cells made from human stem cells to develop an implant that senses and manages blood sugar levels by reacting with the right quantity of insulin at an offered time.
Veiseh, an assistant teacher of bioengineering, has actually invested more than a years establishing biomaterials that secure implanted cell treatments from the body immune system. Miller, an associate teacher of bioengineering, has actually invested more than 15 years looking into strategies to 3D print tissues with vasculature, or networks of capillary.
“If we really want to recapitulate what the pancreas normally does, we need vasculature,” Veiseh stated. “And that’s the purpose of this grant with JDRF. The pancreas naturally has all these blood vessels, and cells are organized in particular ways in the pancreas. Jordan and I want to print in the same orientation that exists in nature.”
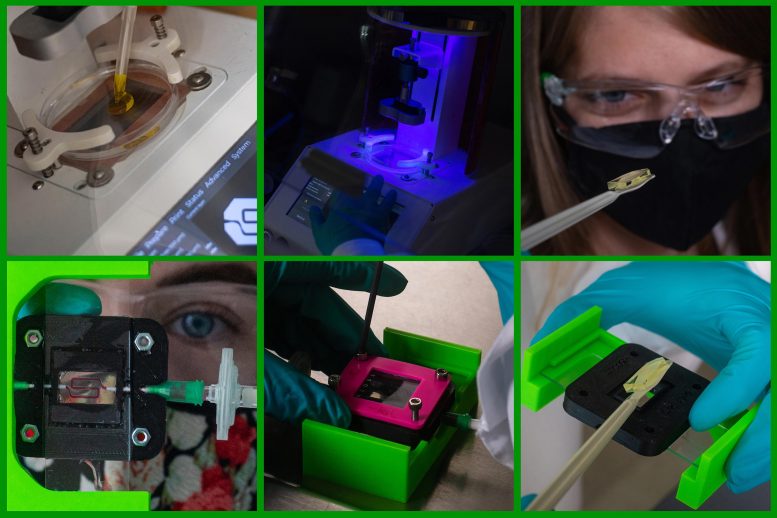
To 3D print vascularized hydrogels that can be developed into living tissue, Rice University bioengineers utilize (leading left) a nontoxic liquid polymer that is (leading middle) strengthened one layer at a time by blue light. Yellow food coloring takes in the light, enabling the development of passages for streaming blood. Postdoctoral scientist Kristen Means (leading right) shows a printed hydrogel that was protected (bottom right and middle) in a plastic real estate for college student Madison Royse’s (bottom left) blood-flow presentation utilizing liquid color. Credit: Photos by Jeff Fitlow/Rice University
Type 1 diabetes is an autoimmune illness that triggers the pancreas to stop producing insulin, the hormonal agent that manages blood-sugar levels. About 1.6 million Americans cope with Type 1 diabetes, and more than 100 cases are detected every day. Type 1 diabetes can be handled with insulin injections. But stabilizing insulin consumption with consuming, workout and other activities is hard. Studies quote that less than one-third of Type 1 diabetics in the U.S. regularly accomplish target blood sugar levels.
Veiseh’s and Miller’s objective is to reveal their implants can correctly control blood sugar levels of diabetic mice for a minimum of 6 months. To do that, they’ll require to offer their crafted beta cells the capability to react to quick modifications in blood sugar level levels.
“We must get implanted cells in close proximity to the bloodstream so beta cells can sense and respond quickly to changes in blood glucose,” Miller stated.
Ideally, insulin-producing cells will disappear than 100 microns from a capillary, he stated.
“We’re using a combination of pre-vascularization through advanced 3D bioprinting and host-mediated vascular remodeling to give each implant several shots at host integration,” Miller stated.
The insulin-producing cells will be secured with a hydrogel solution established by Veiseh, who is likewise a Cancer Prevention and Research Institute of TexasScholar The hydrogel product, which has actually shown reliable for encapsulating cell treatments in bead-sized spheres, has pores little enough to keep the cells inside from being assaulted by the body immune system however big enough to permit passage of nutrients and life-giving insulin.
“Blood vessels can go inside of them,” Veiseh stated of the hydrogel compartments. “At the same time, we have our coating, our small molecules that prevent the body from rejecting the gel. So it should harmonize really well with the body.”
If the implant is too sluggish to react to high or low blood sugar level levels, the hold-up can produce a roller coaster-like result, where insulin levels consistently fluctuate to hazardous levels.
“Addressing that delay is a huge problem in this field,” Veiseh stated. “When you give the mouse — and ultimately a human — a glucose challenge that mimics eating a meal, how long does it take that information to reach our cells, and how quickly does the insulin come out?”
By integrating capillary in their implant, he and Miller wish to permit their beta-cell tissues to act in such a way that more carefully imitates the natural habits of the pancreas.