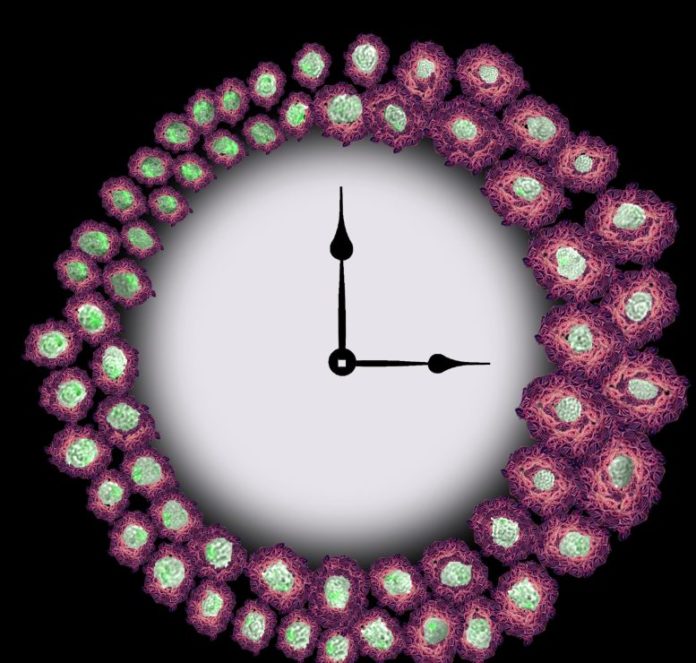
Image Caption: The picture of a clock with brightfield macrophage photos round it reveals how circadian adjustments of cell floor heparan sulfate proteoglycans, proven in pink, impedes phagocytosis of fluorescently labeled amyloid-beta, proven in inexperienced. As time goes on, and we have now a discount in heparan sulfate proteoglycans, we see a rise in phagocytosis, demonstrated by the brilliant inexperienced cells proven on the left of the clock. This picture was made utilizing our fluorescent microscopy cell photos with an inventive rendering of the heparan sulfate proteoglycans from the app, Wombo. The clock was made utilizing photoshop and clip artwork. Credit: Gretchen Clark, made utilizing Wombo (CC-BY 4.0)
The findings present a mechanism that hyperlinks Alzheimer’s disease with circadian rhythm disruptions.
Researchers report that the immune cells responsible for clearing away a key protein that builds up in the brains of patients with Alzheimer’s disease operate according to daily circadian rhythms. The discovery, reported by Jennifer Hurley of Rensselaer Polytechnic Institute and colleagues in a new study publishing today (February 10th, 2022) in the journal PLOS Genetics, provides a potential explanation for the link between Alzheimer’s disease and disruptions to a person’s sleep cycle.
Alzheimer’s disease is known to be associated with disruptions in circadian rhythms, the 24-hour cycle that controls many aspects of human behavior and physiology. For example, sleep disruptions begin years before symptoms of Alzheimer’s disease appear and are linked to more severe symptoms and a higher risk of developing the disease.
In the new paper, researchers investigated a molecular mechanism potentially responsible for the connection between Alzheimer’s disease and circadian rhythms. They measured the activity of immune cells responsible for clearing away proteins called amyloid-beta that build up as plaques in the brains of people with Alzheimer’s disease. Using cultures of these cells grown in the lab, they discovered that the immune cells clear away the amyloid-beta on an oscillating daily cycle controlled by circadian rhythms. However, when cells lost that rhythm, the daily cycle disappeared. They further established that the underlying cause of this oscillation was changes in the number of molecules of a certain protein, heparan, on the cell’s surface. The protein they identified responds to circadian rhythms and previously had been shown to play a role in clearing amyloid-beta proteins.
The new findings uncover a mechanism that links the disruption of circadian rhythms to Alzheimer’s disease. The study further highlights the role of immune cells in this relationship. While more studies will be necessary, the new findings present the possibility that, if the daily clearance of amyloid-beta proteins through this mechanism can be maintained, patients may be less likely to develop Alzheimer’s disease and to exhibit less severe symptoms.
Hurley adds, “Understanding how our circadian rhythms can regulate cell-surface heparan levels to control the build-up of amyloid-beta may lead to the development of chronotherapeutics that alleviate the symptoms of Alzheimer’s Disease as well as other inflammatory diseases.”
Reference: “Circadian control of heparan sulfate levels times phagocytosis of amyloid beta aggregates” by Clark GT, Yu Y, Urban CA, Fu G, Wang C, Zhang F, et al., 10 February 2022, PLoS Genetics.
DOI: 10.1371/journal.pgen.1009994
Funding: This work was supported by an NIH-National Institute of Biomedical Imaging and Bioengineering Grant U01EB022546 (to J.M.H), an NIH-National Institute of General Medical Sciences Grant R35GM128687 (to J.M.H.), an National Science Foundation CAREER Award 2045674 (to J.M.H.), National Institutes of Health grants 1RF1AG069039 (to C.W.), DK111958 and CA231074 (to R.J.L.), Rensselaer Polytechnic Startup funds (to J.M.H.), a gift from the Warren Alpert Foundation (to J.M.H.), and a NIH-National Institute of Aging T32 Fellowship AG057464 (to G.T.C.). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.