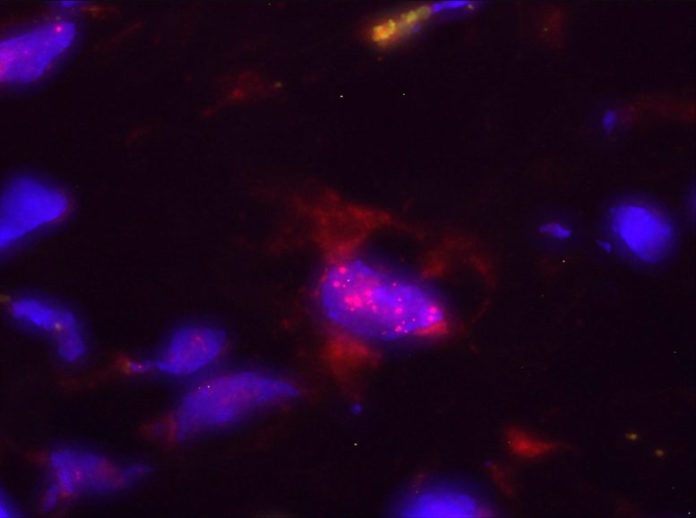
In red, Bacteroides, among the microbes determined in this work, inside nucleus of a pancreatic cell, in blue. Credit: CNIO
A hereditary signature of 27 microbes in stool specifies the high-risk population for pancreatic ductal adenocarcinoma, the most typical pancreatic cancer, and might be utilized for early detection of the illness.
Pancreatic cancer is not one of the most often detected cancers, however it is among the most deadly due to its early regional extension and metastatic behaviour. Some of the factors for this high casualty rate are late medical diagnosis of the illness, particularly given that signs are unspecific and appear rather late, and minimal healing alternatives.
Using client samples offered by a variety of scientific partners, scientists from the Spanish National Cancer Research Centre (CNIO), led by Núria Malats, and the European Molecular Biology Laboratory (EMBL) in Heidelberg, led by Peer Bork, have actually discovered a molecular signature of 27 microbes in stool samples that might anticipate whether clients are at high danger of pancreatic ductal adenocarcinoma, the most typical pancreatic cancer, and even identify clients with earlier phases of the illness.
A patent has actually been obtained to establish a pancreatic cancer diagnostic package that identifies these microbial genomes in stool samples in a fast, non-invasive, and budget-friendly method. The research study was released today in the journal Gut, among the most prominent journals in the fields of gastroenterology and hepatology.
Detecting pancreatic cancer early
The signs of pancreatic cancer are quiet and typically appear in the late phases of the illness, when growths typically can not be gotten rid of through surgical treatment. Therefore, there is an immediate requirement for non-invasive, particular, and budget-friendly tests that have the ability to discover the illness early and enhance client survival.
“In many cases, once pancreatic cancer is detected, it is too late. We need to diagnose the disease at a much earlier stage, before symptoms appear. To do this, we need to identify and define the population at risk and have good screening tests to detect the cancer when it is still curable,” the scientists mentioned.

CNIO scientist NúriaMalats Credit: Laura M. Lombard ía. CNIO
Recent information recommend that the microbes that exist together with cells in the body– the microbiome– might contribute in the origin and advancement of pancreatic ductal adenocarcinoma.
To research study this possible relationship in depth, the scientists carried out a special case-control research study with 136 people (57 recently detected clients, 50 controls, and 27 clients with persistent pancreatitis) who were deeply defined at epidemiological and scientific levels and from whom samples of saliva, feces, and pancreatic tissue were required to evaluate their microbiome. The topics were hired from 2 Spanish health centers in Madrid (Ramon y Cajal Hospital) and Barcelona (Vall Hebron Hospital).
The most detailed research study of the microbiome in pancreatic cancer
Contrary to typical belief, the oral microbiome was not discovered to be connected with pancreatic cancer however fecal microorganisms were. “Sophisticated biostatistical and bioinformatics analyses have allowed us to construct a signature of 27 stool-derived microbes, mostly bacteria, that discriminates very well between cases with pancreatic cancer and controls, both in their most advanced and earliest stages,” stated Malats andBork This gene signature was verified in an independent research study performed in 2 German centers, Frankfurt (Goethe University Hospital) and Erlangen (University Clinic Erlangen), and in 5792 fecal metagenomes from 25 research studies in 18 nations. It is presently being studied in a Japanese population.
However, pancreatic cancer is an illness with an extremely complicated etiology and several danger aspects such as age, weight problems, diabetes, persistent pancreatitis, cigarette smoking, high alcohol intake, blood type, and household history of cancer. To prevent predispositions and to make sure that the microorganisms determined are connected with pancreatic cancer and not with weight problems, diabetes, or other danger aspects, the authors managed for these scientific and market variables in the analysis. “This level of analysis is unprecedented in pancreatic cancer metagenome studies,” the private investigators stated.
As the scientists compose in the pages of Gut, the high predictive worth of this stool gene signature might work as a biomarker to specify the population at danger and, if verified in scientific trials, it might be utilized for early medical diagnosis of pancreatic cancer. “Currently, screening programs are targeted to families with pancreatic cancer aggregation, which represent only 10% of the burden of the disease. The inclusion in these screening programs of a stool analysis to identify the identified microbial signature could help to detect the rest of the population at risk,” they included.
Reference: “A Fecal Microbiota Signature with High Specificity for Pancreatic Cancer” by Kartal et al., 8 March 2022, Gut
DOI: 10.1136/ gutjnl-2021-324755
This research study has actually been performed in partnership with the CNIO Epithelial Carcinogenesis Group led by Paco Real, the CNIO Molecular Cytogenetics Unit led by Sandra Rodr íguez, the Ram ón y Cajal University Hospital Oncological Department led by Alfredo Carrato, the Vall d’ Hebron University Hospital Digestive Disease Department with Xavier Molero, the Translational Hepatology Section in Goethe University Hospital led by Jonel Trebicka, and the group of Stephan Kersting in University Clinic Erlangen.
This research study has actually been moneyed by the World Cancer Research, the European Research Council, the European Regional Development Fund, Spanish Ministry of Science and Innovation, the Carlos III Institute of Health, AESPANC-ACANPAN (Carmen Delgado and Miguel Pérez-Mateo grant) and the European Union (#018771- MOLDIAG-PACA, #259737- CANCERALIA).