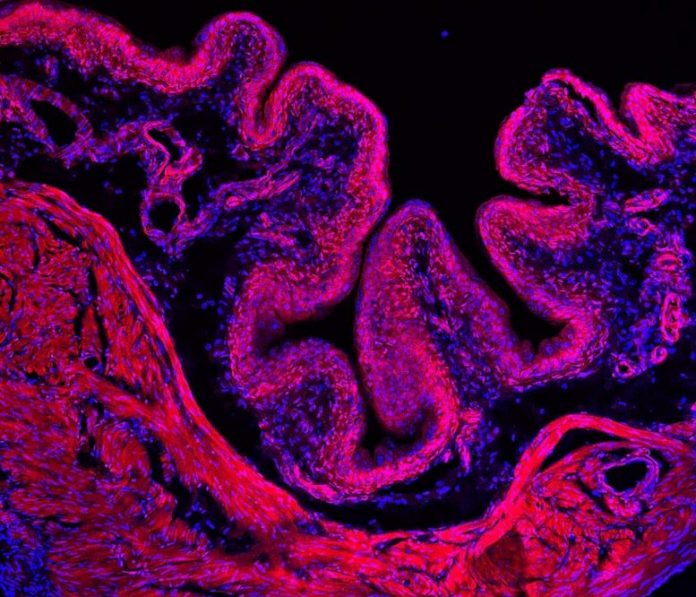
Researchers found that a gene called PIEZO2 might assist us sense when our bladders are complete, and it is time to urinate. Above is an example of a mouse bladder utilized in the research study. Credit: Patapoutian laboratory, Scripps Researcher Institute
In a National Institutes of Health-moneyed research study including both mice and clients who belong to an NIH Clinical Center trial, scientists found that a gene, called PIEZO2, might be accountable for the effective desire to urinate that we generally feel numerous times a day. The results, released in Nature, recommend that the gene assists a minimum of 2 various kinds of cells in the body sense when our bladders are complete and require to be cleared. These results likewise broaden the growing list of recently found senses under the gene’s control.
“Urination is essential for our health. It’s one of the primary ways our bodies dispose of waste. We show how specific genes and cells may play critical roles in initiating this process,” stated Ardem Patapoutian, Ph.D., teacher, Scripps Research Institute, La Jolla, CA and a senior author of the paper. “We hope that these results provide a more detailed understanding of how urination works under healthy and disease conditions.”
Urine is produced when the kidneys extract waste and excess water from the blood and send it to the bladder. Over time, it fills and broadens like a balloon, putting stress on the bladder muscles. Then, at a specific point, the body senses that it is reaching a limitation, which sets off the desire to urinate.
The PIEZO2 gene includes guidelines for making proteins that are triggered when cells are extended or squeezed. In this research study, the scientists discovered that clients who are born with a hereditary shortage in PIEZO2 have difficulty noticing bladder filling while experiments in mice recommended the gene plays 2 crucial functions in this procedure. It might assist specific bladder cells assess growth while likewise stimulating nerve cells to pass on stress signals to the remainder of the nerve system.
The research study was a cooperation in between Dr. Patapoutian’s group and scientists operating in NIH laboratories led by Alex Chesler, Ph.D., senior private investigator, at the NIH’s National Center for Complementary and Integrative Health (NCCIH) and a senior author of the paper, and Carsten Bönnemann, M.D., senior private investigator at the NIH’s National Institute of Neurological Disorders and Stroke (NINDS).
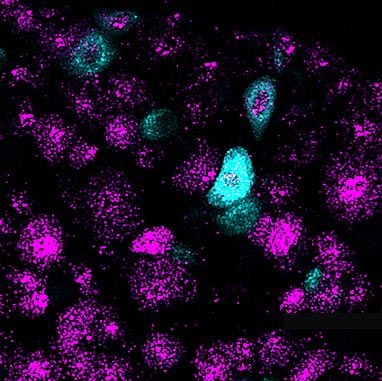
The PIEZO2 gene might assist dorsal root ganglion nerve cells pass on complete bladder signals to the brain. Above is an image of mouse DRGs colored purple. The PIEZO2 gene is colored light blue. Credit: Patapoutian laboratory, Scripps Researcher Institute
In 2010, Dr. Patapoutian’s group found the PIEZO2 gene in addition to a comparable gene called PIEZO1 in a line of mouse brain growths. Before then, researchers understood of just a couple of unusual examples from flies, worms, and mice in which a gene assisted tissue, such as hairy skin cells, sense modifications fit and pressure. Since the discovery, Dr. Patapoutian’s group and others have actually mostly displayed in mice that the PIEZO2 gene might play lots of functions throughout the body consisting of managing the sense of touch, vibration, discomfort, and proprioception, the unconscious awareness of one’s body in area.
More just recently Dr. Patapoutian’s and Dr. Chesler’s groups had actually been checking out whether PIEZO2 contributed in urination.
“There were a lot of reasons to think that PIEZO2 could be important for urination. Theoretically, it made sense as it is a pressure sensor for other internal sensory processes,” stated Kara L. Marshall, Ph.D., a post-doctoral fellow on Dr. Patapoutian’s group and the lead author of the research study.
Then in 2015, an advancement occurred. The NIH scientists found individuals who were born with disabling anomalies in their PIEZO2 genes. Initial assessments of these PIEZO2 lacking people at the NIH’s Clinical Center replicated a few of the mouse results. They had no sense of proprioception and might not feel some types of touch and discomfort. They likewise had something else in typical.
“We were really struck by what we heard during background interviews with patients and their families. Almost everyone mentioned that the patients had problems with urination. As children, they had trouble potty training. They would often have urinary tract infections. And most of them follow a daily urination schedule,” stated Dimah Saade, M.D., a scientific fellow on Dr. Bönnemann’s group and an author of the paper. “After seeing a consistent pattern, we decided to take a closer look.”
The scientists taken a look at medical records, carried out ultrasound scans, administered surveys, and carried out in-depth interviews with 12 clients, 5 to 43 years of age, and their households.
Nearly all the clients declared they might go a whole day without feeling the requirement to urinate and many urinated less than the regular 5 to 6 times each day. In truth, 3 clients reported just going one or two times a day. Five clients reported that when they lastly do want, it begins as an abrupt desire. Seven clients reported that the act of urinating was challenging. They either needed to await it to occur or required to push their lower abdominal area for it to begin.
“These results strongly suggested that PIEZO2 plays a role in urination,” stated Dr. Marshall. “We wanted to know how it may do this.”
In-depth experiments in mice assisted them resolve this concern.
Initially, the scientists discovered that the PIEZO2 gene was extremely active in a couple of dorsal root ganglion (DRG) nerve cells that send out nerve signals from the mouse bladder to the brain. Aided by an innovative, real-time imaging system, they saw that the cells illuminated with activity when a mouse’s bladder filled with fluid. They likewise discovered that the PIEZO2 gene was switched on in some “umbrella” cells which are discovered amongst the cells that line the within a bladder.
“These were the first clues to understanding where in the urinary tract PIEZO2 worked. They suggested that it may help control the bladder,” stated Nima Ghitani, Ph.D., a post-doctoral fellow in Dr. Chesler’s laboratory and an author of the research study.
Next, they discovered that erasing the gene from the nerve cells and umbrella cells not just minimized the cells’ actions to bladder filling however likewise triggered the mice to have issues with urination. The mutant mice revealed some indications of incontinence and urinated arbitrarily in their cages rather of in a corner as seen with control mice. Meanwhile, mutant mouse bladders needed more fluid and higher pressure than regular to activate urination which was similar to the client reports.
They likewise discovered that erasing the gene from the 2 cell types had longer enduring results. For circumstances, the muscles of the mutant bladders were thicker than controls, recommending the loss of experience renovated the bladder.
“Neurologists have always known that there’s a strong link between the nervous system and bladder control, both on a conscious as well as on an automatic level,” stated Dr. Bönnemann. “Our patients together with the results in the mouse models teach us how the loss of the critical sensor PIEZO2 profoundly disrupts the wiring behind normal bladder control, ultimately reshaping the bladder itself.”
Finally, the scientists discovered that erasing the PIEZO2 gene from either the umbrella cells or the DRG nerve cells produced comparable outcomes as erasing it from both cell types all at once. Eliminating the gene from either cell extended the time that mice would take in the past feeling the requirement to squeeze their bladders and it increased the pressure used throughout each capture.
“Our results show how the PIEZO2 gene tightly coordinates urination,” stated Dr. Chesler. “This is a major advance in our understanding of interoception – or the sense of what’s going inside our bodies.”
In the future, the scientists will continue to analyze the function PIEZO2 plays in urination and other interoceptive senses while likewise checking out the medical ramifications of their discovery for the millions struggling with urinatory control issues.
Reference: “PIEZO2 in sensory neurons and urothelial cells coordinates urination” by Kara L. Marshall, Dimah Saade, Nima Ghitani, Adam M. Coombs, Marcin Szczot, Jason Keller, Tracy Ogata, Ihab Daou, Lisa T. Stowers, Carsten G. Bönnemann, Alexander T. Chesler and Ardem Patapoutian, 14 October 2020, Nature.
DOI: 10.1038/s41586-020-2830-7
These research studies were supported by the NINDS and NCCIH departments of intramural research study, NIH grants (NS105067, NS108439, DK121494), and the Howard Hughes Medical Institute.
NINDS is the country’s leading funder of research study on the brain and nerve system. The objective of NINDS is to look for essential understanding about the brain and nerve system and to utilize that understanding to lower the problem of neurological illness.