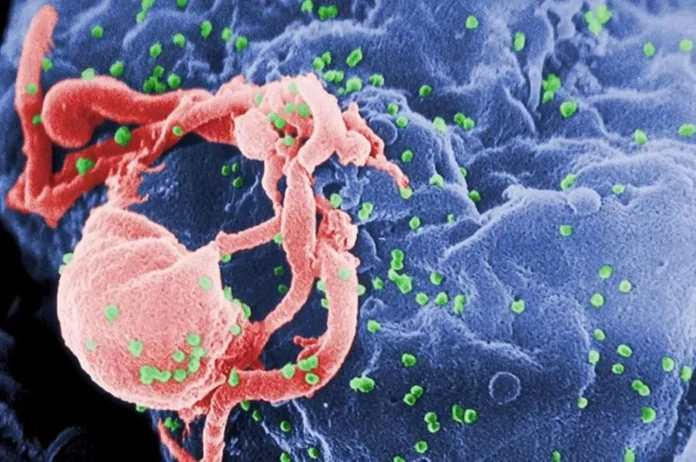
Image of HIV. Credit: CDC/ C. Goldsmith, P. Feorino, E. L. Palmer, W. R. McManus
New analysis reveals why comorbidities persist in individuals residing with HIV, regardless of suppressing the virus by way of remedy.
People residing with HIV usually undergo from continual irritation, despite the fact that antiretroviral remedy has made HIV a manageable illness. This can put them at an elevated danger of growing comorbidities similar to heart problems and neurocognitive dysfunction, which may make a major impression on the longevity and high quality of their lives. Now, a brand new examine printed within the journal Cell Reports on November 14 explains why continual irritation could also be taking place and the way suppression and even eradication of HIV within the physique could not resolve it.
“This research highlights the importance of physicians and patients recognizing that suppressing or even eliminating HIV does not eliminate the risk of these dangerous comorbidities.” — Michael Bukrinsky
In the examine, scientists from the George Washington University display how an HIV protein completely alters immune cells in a means that causes them to overreact to different pathogens. When the protein is launched to immune cells, the researchers discovered that genes in these cells related to irritation activate, or develop into expressed. These pro-inflammatory genes stay expressed, even when the HIV protein is not within the cells. This “immunologic memory” of the unique HIV an infection is why individuals residing with HIV are vulnerable to extended irritation, placing them at higher danger for growing heart problems and different comorbidities, in accordance with the researchers.
“This research highlights the importance of physicians and patients recognizing that suppressing or even eliminating HIV does not eliminate the risk of these dangerous comorbidities,” Michael Bukrinsky, professor of microbiology, immunology, and tropical drugs at GW’s School of Medicine and Health Science and lead writer on the examine, mentioned. “Patients and their doctors should still discuss ways to reduce inflammation and researchers should continue pursuing potential therapeutic targets that can reduce inflammation and co-morbidities in HIV-infected patients.”
For the examine, the analysis staff remoted human immune cells in vitro and uncovered them to the HIV protein Nef. The quantity of Nef launched to the cells is much like the quantity present in about half of HIV-infected individuals taking antiretrovirals whose HIV load is undetectable. After a time frame, the researchers launched a bacterial toxin to generate an immune response from the Nef-exposed cells. Compared to cells that weren’t uncovered to the HIV protein, the Nef-exposed cells produced an elevated degree of inflammatory proteins, known as cytokines. When the staff in contrast the genes of the Nef-exposed cells with the genes of the cells not uncovered to Nef, they recognized pro-inflammatory genes that had been in a ready-to-be-expressed standing on account of the Nef publicity.
These findings might assist clarify why sure comorbidities persist following different viral infections, together with COVID-19, Bukrinsky said.
“We’ve seen this pro-inflammatory immunologic memory reported with other pathogenic agents and often referred to as ‘trained immunity,’” Bukrinsky explains. “While this ‘trained immunity’ evolved as a beneficial immune process to protect against new infections, in certain cases it may lead to pathological outcomes. The ultimate effect depends on the length of this memory, and extended memory may underlie long-lived inflammatory conditions like we see in HIV infection or long COVID.”
Reference: “Extracellular vesicles carrying HIV-1 Nef induce long-term hyperreactivity of myeloid cells” by Larisa Dubrovsky, Beda Brichacek, N.M. Prashant, Tatiana Pushkarsky, Nigora Mukhamedova, Andrew J. Fleetwood, Yangsong Xu, Dragana Dragoljevic, Michael Fitzgerald, Anelia Horvath, Andrew J. Murphy, Dmitri Sviridov and Michael I. Bukrinsky, 14 November 2022, Cell Reports.
DOI: 10.1016/j.celrep.2022.111674
The National Institute of Health’s National Heart, Lung, and Blood Institute supported this research.