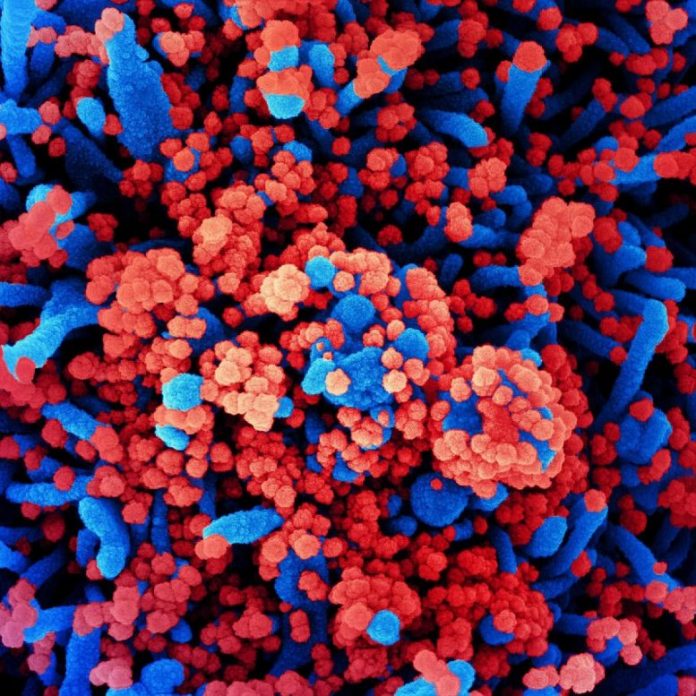
Colorized scanning electron micrograph of a cell (blue) greatly contaminated with SARS-CoV-2 infection particles (red), separated from a client sample. Image recorded at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID
A National Institutes of Health medical trial assessing the security and efficiency of hydroxychloroquine for the treatment of grownups with coronavirus illness 2019 (COVID-19) has actually officially concluded that the drug supplies no medical advantage to hospitalized clients. Though discovered not to trigger damage, early findings in June when the trial was stopped suggested that the drug was not enhancing results in COVID-19 clients. Final information and analyses of the trial, which was moneyed by the National Heart, Lung, and Blood Institute (NHLBI), part of NIH, was released online on November 9, 2020, in the Journal of the American Medical Association.
The trial, called Outcomes Related to COVID-19 treated with Hydroxychloroquine amongst Inpatients with symptomatic Disease (ORCHID), started after laboratory research studies and initial reports recommended that hydroxychloroquine — frequently utilized to deal with malaria and rheumatic conditions like arthritis — may have guarantee in dealing with SARS-CoV-2, the infection that triggers COVID-19.
The Prevention and Early Treatment of Acute Lung Injury (PETAL) Clinical Trials Network of NHLBI began the trial in April at 34 health centers throughout the United States and registered 479 of the anticipated 510 clients. By June, initial proof suggested hydroxychloroquine was not likely to use any advantage.
NIH authorities stated the mindful style, application, and oversight of the research study was crucial to its outcomes, in addition to the suggestion by an information and security tracking board (DSMB) to stop the trial early.
“Having a rigorously designed clinical trial that captured patient-centered, clinically meaningful outcomes was critical to reaching the unequivocal conclusions about the use of hydroxychloroquine in COVID-19. ORCHID shows that hydroxychloroquine does not improve clinical outcomes in hospitalized COVID-19 patients,” stated James P. Kiley, Ph.D., director, Division of Lung Diseases at NHLBI. “We hope this clear result will help practitioners make informed treatment decisions and researchers continue their efforts pursuing other possible safe and effective treatments for patients suffering with this disease.”
The ORCHID trial registered individuals in between April 2 and June 19 who were an average age of 57. They consisted of 290 Hispanic and Black individuals and 212 woman individuals. All individuals got medical care as shown for their condition. Participants were arbitrarily designated to a treatment group and gotten 10 dosages of either hydroxychloroquine or a placebo over 5 days. Researchers then examined each client’s medical status 14 days after being designated to a treatment group. They utilized a seven-category scale varying from one (death) to 7 (released from the medical facility and able to carry out typical activities). Researchers likewise determined 12 extra results, consisting of death that happened 28 days after the individuals’ project to a treatment group.
At day 14, those who got hydroxychloroquine and those who got a placebo had a comparable health status, with many individuals in both groups released from the medical facility and able to carry out a series of activities. The variety of individuals in both treatment groups who passed away at day 14 was likewise comparable. At day 28, 25 of 241 clients in the hydroxychloroquine group and 25 of 236 clients in the placebo group had actually passed away.
“The finding that hydroxychloroquine is not effective for the treatment of COVID-19 was consistent across patient subgroups and for all evaluated outcomes, including clinical status, mortality, organ failures, duration of oxygen use, and hospital length of stay,” stated Wesley Self, M.D., M.P.H., emergency situation medication doctor at Vanderbilt University Medical Center and PETAL Clinical Trials Network private investigator who led the ORCHID trial. He likewise kept in mind that the finding followed comparable trials in the United Kingdom and Brazil.
“Our diverse teams of clinicians and research staff worked nimbly, under extremely difficult circumstances to accomplish what NIH and the PETAL Network do best: ‘gold standard’ studies of important questions for patients suffering from life-threatening conditions,” stated Samuel M. Brown, M.D., M.S., a crucial care doctor at Intermountain Healthcare and PETAL Network private investigator who assisted lead the trial. “While we hoped that hydroxychloroquine would help, even this is an important result as we work together to find effective treatments for COVID-19.”
As of November 9, 2020, the Centers for Disease Control and Prevention has actually reported more than 9.9 million cases of COVID-19 and more than 230,000 deaths in the United States. Many other randomized medical trials are presently assessing the efficiency and security of other representatives versus a placebo in the immediate race for efficient treatments to deal with COVID-19.
Reference: “Effect of Hydroxychloroquine on Clinical Status at 14 Days in Hospitalized Patients With COVID-19A Randomized Clinical Trial” by Wesley H. Self, MD, Miles Per Hour; Matthew W. Semler, MD; Lindsay M. Leither, DO,; Jonathan D. Casey, MD, MSc; Derek C. Angus, MD, Miles Per Hour; Roy G. Brower, MD; Steven Y. Chang, MD, PhD; Sean P. Collins, MD; John C. Eppensteiner, MD; Michael R. Filbin, MD; D. Clark Files, MD; Kevin W. Gibbs, MD; Adit A. Ginde, MD, Miles Per Hour; Michelle N. Gong, MD, MS; Frank E. Harrell Jr, PhD; Douglas L. Hayden, PhD; Catherine L. Hough, MD, MSc; Nicholas J. Johnson, MD; Akram Khan, MD; Christopher J. Lindsell, PhD; Michael A. Matthay, MD; Marc Moss, MD; Pauline K. Park, MD; Todd W. Rice, MD; Bryce R. H. Robinson, MD, MS; David A. Schoenfeld, PhD; Nathan I. Shapiro, MD, Miles Per Hour; Jay S. Steingrub, MD; Christine A. Ulysse, MS; Alexandra Weissman, MD, Miles Per Hour; Donald M. Yealy, MD; B. Taylor Thompson, MD; Samuel M. Brown, MD, MS,; for the National Heart, Lung, and Blood Institute PETAL Clinical Trials Network, 9 November 2020, Journal of the American Medical Association.
DOI:
The ORCHID trial was moneyed by NIH/NHLBI grants 3 U01 HL123009-06S1, U01HL123009, U01HL122998, U01HL123018, U01HL123023, U01HL123008, U01HL123031, U01HL123004, U01HL123027, U01HL123010, U01HL123033, U01HL122989, U01HL123022, and U01HL123020. Additionally, the research study was supported by the National Center for Advancing Translational Sciences Awards UL1TR001102 and UL1TR002541.