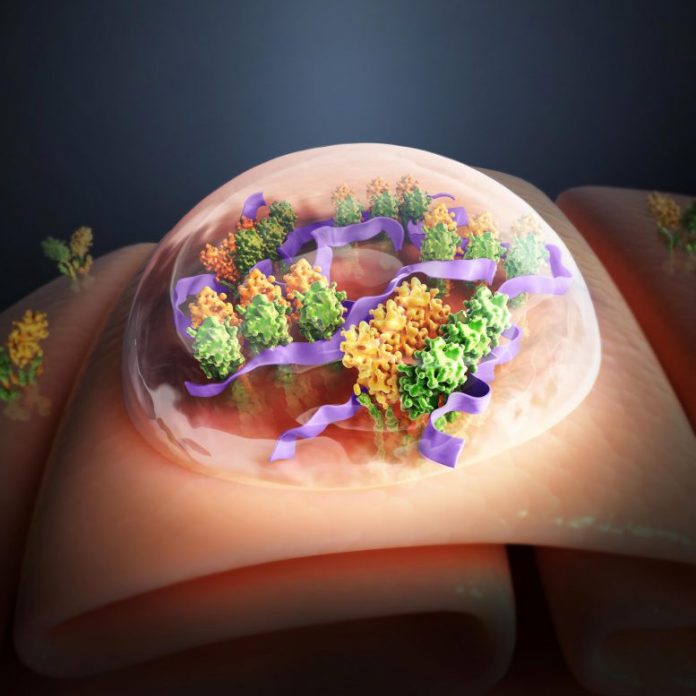
This artist’s making reveals an artificial polymer (purple) that triggers STING proteins (yellow and green themes) for cancer immunotherapy. Credit: Shenyang Zhiyan Science and Technology Co. Ltd.
New immunotherapy drug triggers the body’s natural body immune system to combat cancer.
A brand-new nanoparticle-based drug can improve the body’s natural body immune system and make it more reliable at combating growths, scientists at UT Southwestern have actually revealed. Their research study, released in Nature Biomedical Engineering, is the very first to effectively target the immune particle STING with nanoparticles about one millionth the size of a soccer ball that can change on/off immune activity in reaction to their physiological environment.
“Activating STING by these nanoparticles is like exerting perpetual pressure on the accelerator to ramp up the natural innate immune response to a tumor,” states research study leader Jinming Gao, Ph.D., a teacher in UT Southwestern’s Harold C. Simmons Comprehensive Cancer Center and a teacher of otolaryngology – head and neck surgical treatment, pharmacology, and cell biology.
For more than a years, scientists and pharmaceutical business have actually been racing to establish drugs that target STING, which means “stimulator of interferon genes.” The STING protein, found in 2008, assists moderate the body’s natural body immune system — the collection of immune particles that function as very first responders when a foreign representative flows in the body, consisting of cancer DNA. Research has actually recommended that triggering STING can make the natural body immune system more effective at battling growths or infections. However, arises from earlier medical trials including first-generation substances targeting STING for activation stopped working to show an excellent medical impact.
“A major limitation of conventional small molecule drugs is that after injection into tumors, they are washed out from the tumor site by blood perfusion, which can reduce antitumor efficacy while causing systemic toxicities,” describes Gao.
Jinming Gao, Ph.D. Credit: UT Southwestern Medical Center
Gao and his associates at UTSW found another technique that is various from the earlier or first-generation STING agonist techniques that make use of artificial cyclic dinucleotide to trigger STING in the body. Gao and his group intended to create a polymer — a manmade macromolecule that can self-assemble into nanoparticles — to successfully provide cyclic GMP-AMP (cGAMP), a natural little particle activator of STING, to the protein target. But one polymer they manufactured, PC7A, produced an unforeseen and unique impact: It triggered STING even without cGAMP. The group reported the preliminary lead to 2017, not understanding at the time precisely how PC7A worked; the polymer didn’t look like any other drugs that triggered STING.
In the brand-new paper, Gao’s group revealed that PC7A binds to a various website on the STING particle from understood drugs. Moreover, its impact on the STING protein is various. While existing drugs trigger the protein throughout about 6 hours, PC7A types polyvalent condensates with STING for over 48 hours, triggering a more continual impact on STING. This longer natural immune activation, they revealed, causes a more reliable T cell reaction versus several strong growths. Mice made it through longer and had slower tumor development when they got a mix of PC7A and cGAMP, the scientists discovered.
The polymer likewise has other benefits. When distributing in the blood stream, the polymers exist as little round nanoparticles that do not bind to STING. It’s just when those nanoparticles get in immune cells that they separate, connect to STING, and trigger the immune reaction. That suggests that PC7A may be less most likely to trigger negative effects throughout the body than other STING-targeting drugs, states Gao, although medical trials will be required to show that.
Because PC7A binds to a various website of the STING particle, the substance may operate in clients for whom normal STING-targeting drugs do not. Up to 20 percent of individuals have actually acquired a somewhat various gene for STING; the alternative makes the STING protein resistant to a number of cyclic dinucleotide drugs. Gao and his group showed that PC7A can still trigger cells that reveal these STING versions.
“There’s been a lot of excitement about therapies that target STING and the potential role these compounds could play in expanding the benefits of immunotherapies for cancer patients,” states Gao. “We believe that our new nanotechnology approach offers a way to activate STING without some of the limitations we’ve seen with earlier STING agonist drugs in development.”
Reference: “Polycarbonate-based ultra-pH sensitive nanoparticles improve therapeutic window” by Xu Wang, Jonathan Wilhelm, Wei Li, Suxin Li, Zhaohui Wang, Gang Huang, Jian Wang, Houliang Tang, Sina Khorsandi, Zhichen Sun, Bret Evers and Jinming Gao, 17 November 2020, Nature Communications.
DOI: 10.1038/s41467-020-19651-7
Other UTSW scientists who added to this research study were Suxin Li, Min Luo, Zhaohui Wang, Qiang Feng, Jonathan Wilhelm, Xu Wang, Wei Li, Jian Wang, Agnieszka Cholka, Yang-xin Fu, Baran Sumer, and Hongtao Yu.
This research study was supported by funds from the National Institutes of Health (U54 CA244719) and Mendelson-Young Endowment for Cancer Therapeutics.
Gao holds the Elaine Dewey Sammons Distinguished Chair in Cancer Research, in honor of Eugene P. Frenkel, M.D. at UTSW.