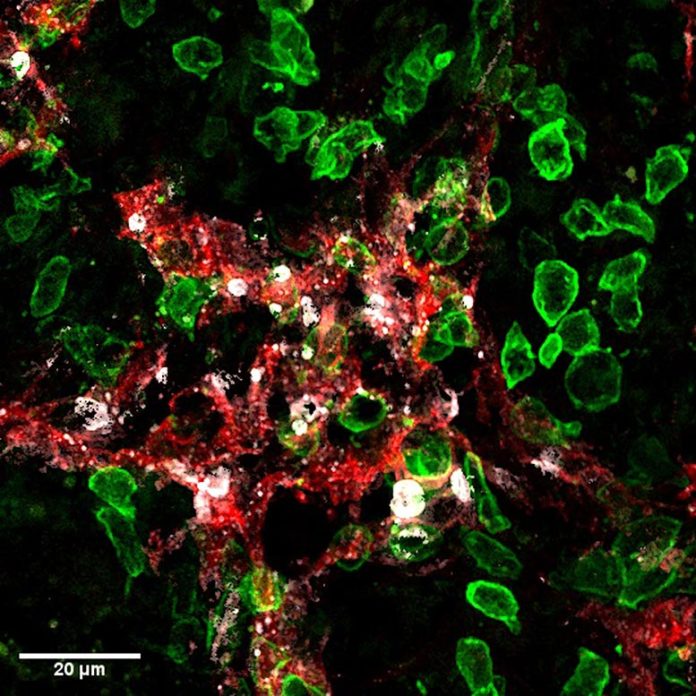
Killer- T cells (green) attack lymphatic vessels (red) in growths and cause their death (cell death marker in white). Credit: UNIGE– Robert Pick/ St éphanie Hugues
University of Geneva researchers highlight the unanticipated result of particular immunotherapies to avoid cancer metastases.
Tumors count on a particular structure, the growth stroma, to grow. This consists of capillary, which supply the nutrients needed for infected cells to increase, in addition to lymphatic vessels, through which they move to metastasize. The development of lymphatic vessels– a system called lymphangiogenesis– around a growth is for that reason of bad diagnosis.
A group of researchers has actually shown how “killer” T-cells utilized in immunotherapy to remove cancer cells can likewise damage growth lymphatic vessels, therefore significantly lowering the threat of transition. Exploiting this synergistic result might increase the effectiveness of treatments versus cancers where lymphangiogenesis is very important, such as colorectal cancer, cancer malignancy, or breast cancer. These arises from scientists at the University of Geneva (UNIGE) can be checked out in the journal Science Advances.
Killer T cells (likewise called a cytotoxic T cell or a cytotoxic T lymphocyte) are a kind of immune cell that can eliminate particular cells, such as foreign cells, cancer cells, and cells contaminated with an infection. Killer T cells can be separated from other blood cells, grown in the lab, and after that administered to a client to eliminate cancer cells. A killer T cell is a kind of leukocyte and a kind of lymphocyte.
The lymphatic system is the primary path through which cancer cells spread out in the body. They very first colonize the guard lymph nodes, then transfer to trigger secondary metastases in other places in the body. However, treatments to obstruct growth lymphangiogenesis have actually up until now been frustrating. “Indeed, they also represent the route for some immune cells, the dendritic cells, to exit from the tumor and activate anti-tumoral killer-T cells,” discusses St éphanie Hugues, Associate Professor in the Department of Pathology and Immunology and in the Geneva Center for Inflammation Research of the UNIGE Faculty of Medicine, who led this work. “We must therefore find a balance in order to inhibit this mechanism without blocking it completely, and thus decipher its mode of action in detail.”
Identifying a special target
To do this, the researchers utilized so-called “killer” T lymphocytes utilized in immunotherapy procedures. “These T-cells are immune cells specifically activated in labs to eliminate tumor cells, before being injected into patients,” discusses Laure Garnier, a junior speaker in St éphanie Hugues’ lab and very first author of this work. “Here, we injected them into mice suffering from melanoma. And if, as expected, the killer lymphocytes destroyed the tumor cells, they also attacked the lymphatic endothelial cells that line the lymphatic vessels.”
Indeed, the damage of cancer cells results in the release of growth antigens. These little malignant parts are then recorded by the lymphatic endothelial cells which, having actually ended up being providers of growth recognition markers, are likewise acknowledged as opponents by the T-cells that assault them. This system, for that reason, interferes with the tumor-associated lymphatic system to substantially lower the threat of transition without obstructing it completely.
The research study group validated these outcomes with other methods, such as vaccination, which intends to enhance the body immune system. “We also observed the destruction of lymphatic endothelial cells, and consequently a decrease in lymph node metastases, thus limiting the risk of secondary metastases. Moreover, as this action only takes place in the tumor microenvironment, no systemic effect is to be feared,” highlights Laure Garnier.
Increasing synergies by selecting the best weapons
How can this result be reinforced without endangering the action of the immune cells, which require the lymphatic vessels to get in the growth? There are numerous choices, such as stepping in as soon as resistance has actually been developed, or in combination with restorative procedures where the body immune system is so strong that restricting lymphangiogenesis would not hinder its function. “Nevertheless, our results show that the most effective approach is to use killer T-cells generated in the laboratory, and therefore ready to attack, in order to bypass the first phase of activation, which can prove problematic,” states St éphanie Hugues.
Immunotherapies stay intricate and are just utilized when conventional treatments have actually shown undetermined. “Even though they are very promising, these therapies are not miracle solutions and often cause severe side effects. This is why we want to understand the smallest biological processes at work,” the authors conclude.
Reference: “IFN-γ–dependent tumor-antigen cross-presentation by lymphatic endothelial cells promotes their killing by T cells and inhibits metastasis” by Laure Garnier, Robert Pick, Julien Montorfani, Mengzhu Sun, Dale Brighouse, Nicolas Liaudet, Thomas Kammertoens, Thomas Blankenstein, Nicolas Page, Jeremiah Bernier-Latamani, Ngoc Lan Tran, Tatiana V. Petrova, Doron Merkler, Christoph Scheiermann and St éphanie Hugues, 8 June 2022, Science Advances
DOI: 10.1126/ sciadv.abl5162