Cell culture research studies reveal increased lung cell entry of the SARS-CoV-2 variations Delta and Delta Plus and decreased inhibition by antibodies.
The introduction of brand-new SARS-CoV-2 variations that can spread out quickly and weaken vaccine-induced resistance threatens completion of the COVID-19 pandemic.
The delta variation (B. 1.6172) emerged in India and consequently spread out worldwide within a brief time duration. Also in Germany, practically all current infections are because of this variation. In addition to Delta, so-called Delta Plus sub-variants have actually been observed, which bring extra anomalies that might make them more unsafe.
A research study group led by Stefan Pöhlmann and Markus Hoffmann from the German Primate Center– Leibniz Institute for Primate Research in Göttingen and associates from the Hannover Medical School, the University of Göttingen Medical Center and the Friedrich-Alexander University of Erlangen- Nürnberg have actually examined why the Delta alternative spreads so effectively and whether Delta Plus infections are more unsafe.
They had the ability to reveal that Delta and Delta Plus contaminate lung cells with greater effectiveness than the initial infection. In addition, among 4 antibodies utilized to deal with COVID-19 was ineffective versus Delta, and Delta Plus was even resistant versus 2 restorative antibodies. Similarly, antibodies produced upon vaccination with the BioNTech-Pfizer and Oxford- AstraZeneca vaccines were likewise less efficient versus Delta and Delta Plus compared to the initial infection. Delta and Delta Plus, on the other hand, were comparably hindered, recommending that Delta Plus might not present a higher threat to immunized individuals than Delta.
Finally, it was discovered that people immunized initially with Oxford- AstraZeneca and after that with BioNTech-Pfizer had substantially more antibodies that hindered Delta than people immunized two times with Oxford- AstraZeneca. The mix of 2 vaccines might therefore cause an especially strong immune defense versus SARS-CoV-2 variations (The Lancet, Cell Reports, Cell Mol Immunol).
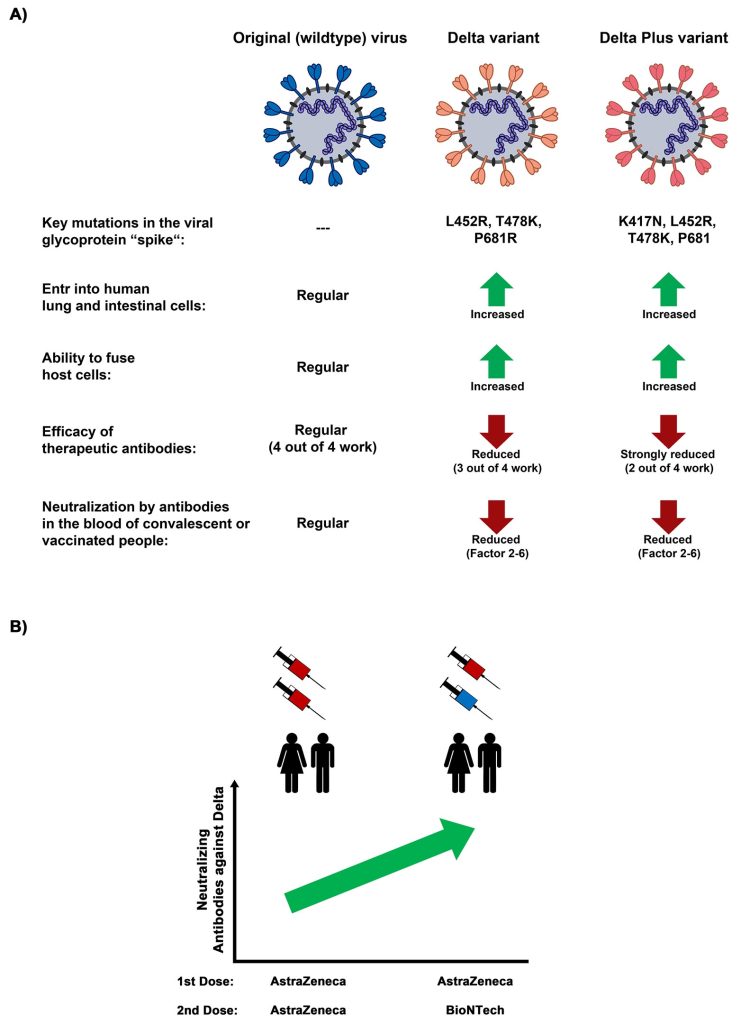
A) Summary of unique residential or commercial properties of SARS-CoV-2 Delta and Delta Plus variations compared to the infection flowing to the start of the pandemic (wildtype infection). B) Heterologous vaccination with Oxford- AstraZeneca’s vector-based vaccine and BioNTech-Pfizer’s mRNA-based vaccine Induces the production of more reducing the effects of antibodies versus the Delta alternative than homologous (two-shot) vaccination with Oxford- AstraZeneca. Credit: Markus Hoffmann
At present, more than 99 percent of SARS coronavirus 2 infections triggered in Germany are because of the Delta variation, according to the Robert KochInstitute Using cell culture experiments, a group of scientists led by Stefan Pöhlmann and Markus Hoffmann had the ability to reveal that Delta is much better at going into lung cells compared to the initial infection (the infection that distributed throughout the early stage of the pandemic). In addition, Delta is much better at merging contaminated lung cells with uninfected cells.
“It is conceivable that by fusing cells in the respiratory tract, the Delta variant may spread more efficiently and induce more damage. This could contribute to a more severe course of COVID-19,” presumes Arora Prerna, researcher at the German Primate Center and very first author of 2 research studies particularly concentrating on the Delta and Delta Plus variations.
Monoclonal antibodies are utilized to deal with COVID-19 These antibodies are proteins that are produced by genetic modification. Unlike our body immune system, which produces a a great deal of various antibodies versus pathogens throughout infection, just specific antibodies or mixes of them are utilized for COVID-19 treatment. The group led by Stefan Pöhlmann and Markus Hoffmann studied 4 of these antibodies. They discovered that Delta is resistant versus the antibody bamlanivimab, while Delta Plus is resistant versus 2 antibodies, bamlanivimab and etesevimab, which are utilized in mix for treatment of COVID-19 clients.
Delta and Delta Plus were less well hindered (reduced the effects of) by antibodies from contaminated and immunized people as compared to the initial infection and this most likely added to the quick spread ofDelta A direct contrast of Delta and Delta Plus revealed that both infections were comparably reduced the effects of. “This means that vaccination likely confers comparable protection against Delta and Delta Plus, and that Delta Plus is not significantly more dangerous than Delta,” states Stefan Pöhlmann.
BioNTech-Pfizer’s vaccine is the most commonly utilized vaccine in Europe, followed by Oxford- AstraZeneca’s vaccine. Due to extremely uncommon adverse effects following vaccination with Oxford- AstraZeneca, it is suggested in Germany and other nations that BioNTech-Pfizer is utilized for the 2nd vaccination shot in individuals who have actually currently gotten a very first shot with Oxford- AstraZeneca. This method is described as heterologous vaccination.
“Our studies show that heterologous vaccination induces significantly more neutralizing antibodies to Delta than two vaccination shots with Oxford-AstraZeneca. Individuals who have received such a heterologous vaccination may have a very good immune protection against Delta and Delta Plus,” states Markus Hoffmann.
“Our results are consistent with the observation that vaccination efficiently protects against development of severe disease after infection with the Delta variant, but frequently fails to completely suppress infection. In light of the efficient protection against severe disease, the goal continues to be a high vaccination rate. This can prevent the health care system from being overwhelmed in case of increased spread of Delta and closely related viruses during the winter months,” states Stefan Pöhlmann.
Reference: “B.1.617.2 enters and fuses lung cells with increased efficiency and evades antibodies induced by infection and vaccination” by Prerna Arora, Anzhalika Sidarovich, Nadine Kr üger, Amy Kempf, Inga Nehlmeier, Luise Graichen, Anna-Sophie Moldenhauer, Martin S. Winkler, Sebastian Schulz, Hans-Martin Jäck, Metodi V. Stankov, Georg M.N. Behrens, Stefan Pöhlmann and Markus Hoffmann, 27 September 2021, Cell Reports
DOI: 10.1016/ j.celrep.2021109825





