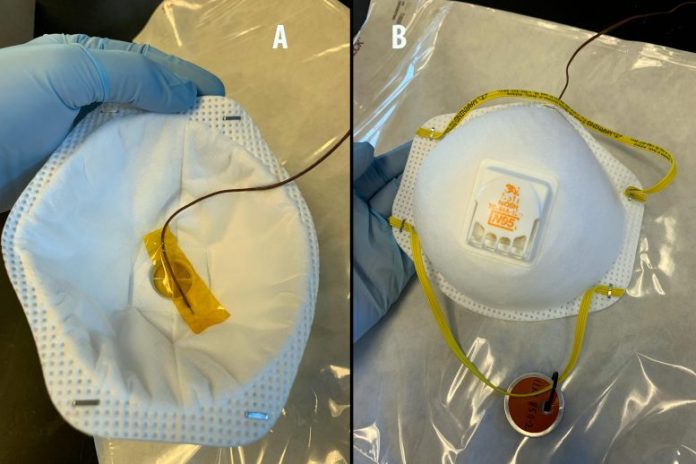
Inner and external view of an N95 mask in between dry heat treatment cycles revealing no contortion of the respirator. A thermocouple is attached to the inner surface area of the respirator with Kapton tape to determine the surface area temperature level of the mask over 10 heating cycles in a basic lab convection box oven. Masks are heat dealt with inside a self-sealing autoclave pouch (background) to avoid dispersion of viral particles from air flow inside the oven. Credit: Trevis Massey/LLNL
Lawrence Livermore National Laboratory (LLNL) scientists are studying methods to securely and quickly get rid of viral risks from N95 respirators, without jeopardizing the gadget’s fit and its capability to filter air-borne particles, so they can be recycled.
As seen throughout the COVID-19 pandemic, a lack of individual protective devices, consisting of surgical masks and respirators, can hamper efforts to assist contaminated clients, along with efforts to safeguard medical companies and very first responders.
N95 respirators are protective gadgets that filter air-borne particles. The “N95” classification implies that the respirator obstructs a minimum of 95 percent of really little (0.3 micrometers or bigger) test particles. They are normally utilized a single time in healthcare settings since the respirators can be polluted when dealing with contaminated clients, thus posturing a danger to caretakers who continue using an infected gadget, along with other clients dealt with by the supplier.
According to Sal Baxamusa, who leads LLNL’s research study group, they are checking out methods to shut off the SARS-CoV-2 infection on N95 respirators utilizing economical tools that are easily offered in medical facilities, along with field settings, to make sure the ongoing schedule of this important resource throughout a crisis.
“In health care settings, it is always preferable to use an N95 respirator just one time. But in emergency situations, additional options may need to be considered,” stated Baxamusa.
LLNL’s group is studying deactivation strategies that quickly get rid of the viral danger, without jeopardizing the method the respirator fits on the user’s face, and without leaving poisonous residue that might hurt users. For example, liquid disinfectants like bleach can harm the filter, and sanitation techniques that depend on ultraviolet light do not permeate deep sufficient to completely decontaminate the filter. Sending masks off website to a main area with advanced decontamination devices might not be useful throughout a crisis, when there is a minimal supply of respirators.
Thermal procedure to shut off infection
The LLNL group is checking the effectiveness of utilizing a thermal procedure, where heat permeates through the external cover of the respirator to shut off the infection on internal parts, consisting of the filtering component. At the exact same time, they are studying whether respirators maintain performance after thermal treatment.
Using a basic lab oven, the group performed preliminary tests relating to how thermal treatment impacts respirator parts that play an essential function in making sure a safe and secure fit on the user’s face, such as the metal nose clip, nose foam and neck straps. Following treatment, they checked the fit of the masks in LLNL’s respirator store and recognized thermal conditions that do not jeopardize the fit.
With these preliminary tests finished, the group is now studying deactivation effectiveness. Using a mouse liver disease infection that belongs to SARS-CoV-2 however does not trigger illness in people, they are examining whether any live infection stays on the filter of an N95 respirator after heat treatment. Following treatment, they will carefully get rid of viral particles from the product and count the variety of transmittable particles that exist.
While thermal treatment does not entirely decontaminate all pathogens, the research study group expects that it can shut off infections.
“We are thrilled to be part of this effort to explore options for field-based reuse of respirators,” stated Bob Maxwell, who leads LLNL’s Materials Science Division. “This type of solution would make it possible to safely reuse respirators during a pandemic, or any other situation where supplies are limited, and front-line health care workers need protection.”
The multidisciplinary research study group consists of products researchers, biologists and engineers who quickly came together throughout LLNL’s minimal operations to study this difficulty and supply lead to a sped up timeframe. In addition to Baxamusa, the group consists of Mihail Bora, Monica Borucki, Eric Duoss, Kyle Fuhrer, Razi Haque, Travis Massey, Samuel Paik and Maxim Shusteff.