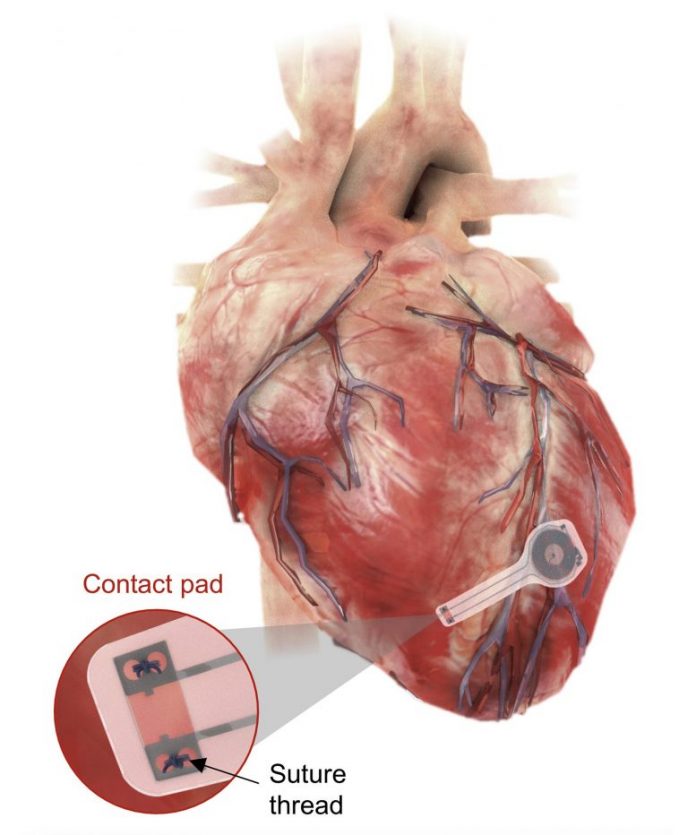
An illustration of the short-term pacemaker installed on myocardial tissue. Credit: Northwestern University/George Washington University
Wireless, completely implantable gadget provides short-lived pacing without needing elimination.
- Bioresorption bypasses requirement to extract non-biodegradable leads, removing extra threat to client
- Pacemaker is from another location powered by near-field interaction procedures
- Researchers checked the gadget throughout a series of big and little animal designs
- Heart cosmetic surgeon: ‘This device will greatly improve a patient’s post-operative course’
Researchers at Northwestern and George Washington universities (GW) have actually established the first-ever short-term pacemaker — a cordless, battery-free, completely implantable pacing gadget that vanishes after it’s no longer required.
The thin, versatile, light-weight gadget might be utilized in clients who require short-lived pacing after heart surgical treatment or while awaiting an irreversible pacemaker. All parts of the pacemaker are biocompatible and naturally take in into the body’s biofluids throughout 5 to 7 weeks, without requiring surgical extraction.
The gadget wirelessly collects energy from an external, remote antenna utilizing near-field interaction procedures — the very same innovation utilized in mobile phones for electronic payments and in RFID tags. This removes the requirement for large batteries and stiff hardware, consisting of wires (or leads). Not just can leads present infections, they likewise can end up being covered in scar tissue, triggering more damage when eliminated.
The research study was released on June 28, 2021, in the journal Nature Biotechnology. The paper shows the gadget’s effectiveness throughout a series of big and little animal designs.
Watch the short-term pacemaker gradually liquify throughout 35 days and beyond. Credit: Northwestern University
“Hardware placed in or near the heart creates risks for infection and other complications,” stated Northwestern’s John A. Rogers, who led the gadget’s advancement. “Our wireless, transient pacemakers overcome key disadvantages of traditional temporary devices by eliminating the need for percutaneous leads for surgical extraction procedures — thereby offering the potential for reduced costs and improved outcomes in patient care. This unusual type of device could represent the future of temporary pacing technology.”
“Sometimes patients only need pacemakers temporarily, perhaps after an open heart surgery, heart attack, or drug overdose,” stated Dr. Rishi Arora, a cardiologist at Northwestern Medicine who co-led the research study. “After the patient’s heart is stabilized, we can remove the pacemaker. The current standard of care involves inserting a wire, which stays in place for three to seven days. These have potential to become infected or dislodged.”
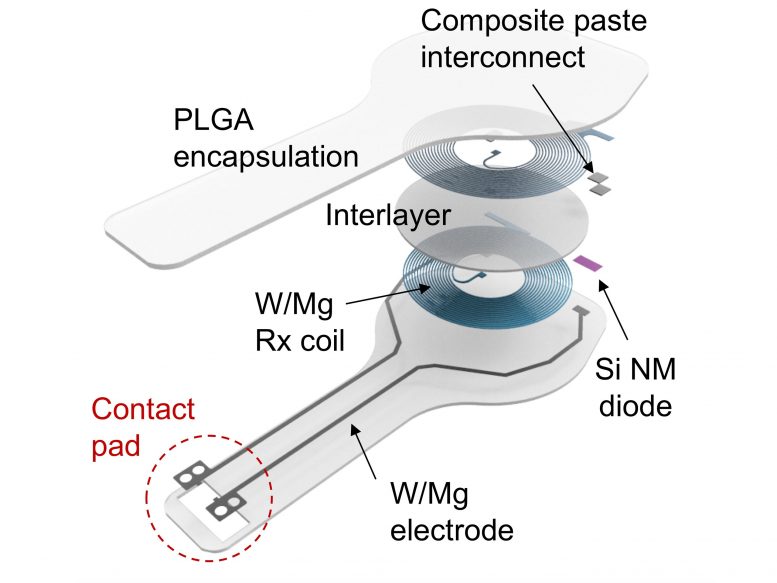
Layered schematic of the gadget, with annotation. Credit: Northwestern University/George Washington University
“The transient electronics platform opens an entirely new chapter in medicine and biomedical research,” stated GW’s Igor Efimov, who co-led the research study with Rogers and Arora. “The bioresorbable materials at the foundation of this technology make it possible to create whole host of diagnostic and therapeutic transient devices for monitoring progression of diseases and therapies, delivering electrical, pharmacological, cell therapies, gene reprogramming and more.”
Rogers is the Louis Simpson and Kimberly Querrey Professor of Materials Science and Engineering, Biomedical Engineering and Neurological Surgery in the McCormick School of Engineering and Feinberg School of Medicine and the director of the Querrey Simpson Institute for Bioelectronics. Arora is a teacher of medication at Feinberg and co-director of the Center for Arrhythmia Research. Efimov is the Alisann and Terry Collins Professor of Biomedical Engineering at GW.
Ditching limiting, dangerous leads
Currently, to establish a short-lived pacing after open heart surgical treatment, cosmetic surgeons need to stitch on short-lived pacemaker electrodes on the heart muscle throughout surgical treatment. These have leads that exit the front of a client’s chest, linking to an external pacing box that provides an existing to manage the heart’s rhythm.
When the short-lived pacemaker is no longer required, doctors eliminate the pacemaker electrodes. Although unusual, possible problems of implanted short-lived pacemakers consist of infection, dislodgement, torn or harmed tissues, bleeding, and embolism.
With Northwestern and GW’s short-term pacemaker, cosmetic surgeons and clients can avoid this possibly dangerous treatment. The completely implantable gadget is light and thin — 250 microns thick and weighing less than half a gram. Soft and versatile, it encapsulates electrodes that gently laminate onto the heart’s surface area to provide an electrical pulse.
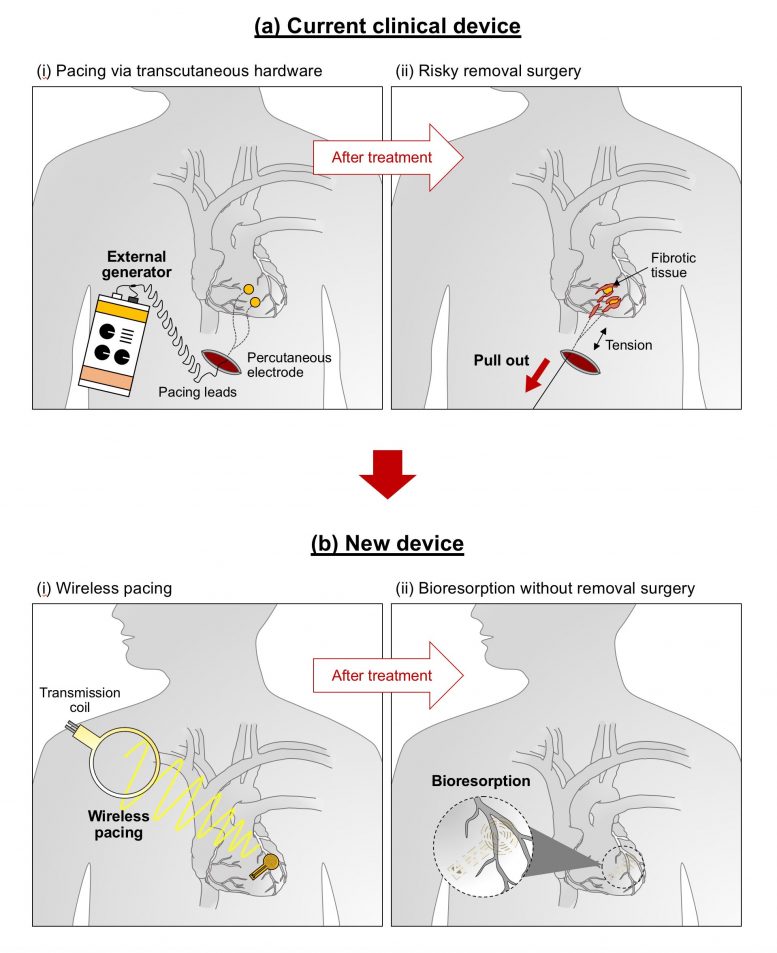
Illustrated contrast of existing innovation versus the brand-new short-term innovation. Credit: Northwestern University/George Washington University
“Instead of using wires that can get infected and dislodged, we can implant this leadless biocompatible pacemaker,” Arora stated. “The circuitry is implanted straight on the surface area of the heart, and we can trigger it from another location. Over a duration of weeks, this brand-new kind of pacemaker ‘dissolves’ or breaks down by itself, consequently preventing the requirement for physical elimination of the pacemaker electrodes. This is possibly a significant triumph for post-operative clients.
“With further modifications, it eventually may be possible to implant such bioresorbable pacemakers through a vein in the leg or arm,” he included. “In this instance, it also may be possible to provide temporary pacing to patients who have suffered a heart attack or to patients undergoing catheter-based procedures, such as trans-catheter aortic valve replacement.”
Prioritizing client convenience
Northwestern Medicine heart cosmetic surgeon Dr. Duc Thinh Pham, who was not included with the research study, thinks of a short-term pacemaker certainly would make his clients more comfy. With existing pacemakers, clients typically feel pain for days after the leads are placed. Then, they need to restrict their motions and activities in order to avoid the leads from removing.
“This transient pacemaker is brilliant,” stated Pham, who has actually carried out more than 2,000 heart surgical treatments throughout his profession. “In addition to addressing the primary issue of occasional post-cardiac surgery patients needing temporary pacing due to blockages or arrhythmias, the device addresses the secondary issue of patient comfort, ability to move freely and rehabilitate. If successful, this device will greatly improve a patient’s post-operative course.”
Disappearing act
This is the 2nd example of bioresorbable electronic medication from the Rogers laboratory, which has actually been studying short-term electronic devices for over a years. In 2018, Rogers and coworkers showed the world’s very first bioresorbable electronic gadget — a naturally degradable implant that speeds nerve regrowth. The group’s bioresorbable gadgets are entirely safe — comparable to absorbable stitches. After completely degrading, the gadgets entirely vanish through the body’s natural biological procedures.
“There is clearly a need for better temporary cardiac pacemakers,” stated Dr. Bradley Knight, the Chester C. and Deborah M. Cooley Distinguished Professor of Cardiology at Feinberg and coauthor of the research study. “When I first learned about the bioresorbable nerve stimulator, I contacted Professor Rogers to explore the possibility of using this technology to pace the heart. He had already started working with Dr. Efimov to develop a small version of a bioresorbable pacemaker as a proof of concept. We then worked with both teams to develop a larger version of a bioresorbable, leadless, cardiac pacemaker that could be effective on a human scale. It’s a great example of what we can create at Northwestern by bridging the expertise in engineering and medicine.”
Depending on the client, a short-lived pacemaker may be required anywhere from a couple days to a number of weeks. By differing the structure and density of the products in the gadget, Rogers’ group can manage the accurate variety of days it stays practical prior to liquifying.
“We build these devices out of different types of safe, bioresorbable materials and in optimized architectures to ensure stable operation over a time period somewhat longer than is clinically necessary,” Rogers stated. “We can tailor the devices to address a broad spectrum of relevant lifetimes. Transient technologies, in general, could someday provide therapy or treatment for a wide variety of medical conditions — serving, in a sense, as an engineering form of medicine.”
Reference: “Fully implantable and bioresorbable cardiac pacemakers without leads or batteries” by Yeon Sik Choi, Rose T. Yin, Anna Pfenniger, Jahyun Koo, Raudel Avila, K. Benjamin Lee, Sheena W. Chen, Geumbee Lee, Gang Li, Yun Qiao, Alejandro Murillo-Berlioz, Alexi Kiss, Shuling Han, Seung Min Lee, Chenhang Li, Zhaoqian Xie, Yu-Yu Chen, Amy Burrell, Beth Geist, Hyoyoung Jeong, Joohee Kim, Hong-Joon Yoon, Anthony Banks, Seung-Kyun Kang, Zheng Jenny Zhang, Chad R. Haney, Alan Varteres Sahakian, David Johnson, Tatiana Efimova, Yonggang Huang, Gregory D. Trachiotis, Bradley P. Knight, Rishi K. Arora, Igor R. Efimov and John A. Rogers, 28 June 2021, Nature Biotechnology.
DOI: 10.1038/s41587-021-00948-x
The paper, “Fully bioresorbable, leadless, battery-free cardiac pacemaker,” was supported by the Leducq Foundation (RHYTHM award), National Institutes of Health (award numbers R01-HL141470, R01-HL140061 and R01-HL125881), the American Heart Association (award number 19PRE34380781, AF SFRN), the National Science Foundation (award number 1842165) and the Ford Foundation. The paper’s co-first authors are Yeon Sik Choi, Rose Yin, Jahyun Koo and Anna Pfenniger.