SARS-CoV-2 utilizes its spike protein to attatch to a host cell.
Therapeutic technique established by Weizmann Institute researchers might spell brand-new hope in the fight versus COVID-19
Even though vaccines might be guiding the world towards a post-pandemic typical, a continuously altering SARS-CoV-2 demands the advancement of reliable drugs. In a brand-new research study released in Nature Microbiology, Weizmann Institute of Science scientists, together with partners from the Pasteur Institute, France, and the National Institutes of Health (NIH), U.S.A., use an unique healing technique to combating the well-known infection. Rather than targeting the viral protein accountable for the infection going into the cell, the group of scientists attended to the protein on our cells’ membrane that allows this entry. Using an innovative synthetic advancement approach that they established, the scientists produced a molecular “super cork” that physically jams this “entry port,” therefore avoiding the infection from connecting itself to the cell and entering it.

Prof GideonSchreiber A brand-new technique for dealing with COVID-19 established by methods of synthetic advancement. Credit: Weizmann Institute of Science
Most possible treatments (and present vaccines) for SARS-CoV-2 target the so-called “spike protein” discovered on the infection’s external envelope. This protein, nevertheless, is susceptible to anomalies that wear down the effectiveness of these treatments. “Since the virus is constantly evolving we have, instead, focused on the non-evolving human receptor called ACE2 that acts as the entry site for the virus,” statesProf Gideon Schreiber of Weizmann’s Biomolecular Sciences Department, who monitored the brand-new research study. This technique is not vulnerable to brand-new emerging infection versions, which is among the primary difficulties in battling the pandemic.
ACE2, connected to the membrane of lung epithelial cells and other tissues, is an enzyme crucial for controling high blood pressure. Therefore, as appealing as it might be to just obstruct this receptor to avoid the entry of SARS-CoV-2, any such technique should not interfere with ACE2’s function. Schreiber, whose laboratory focuses on studying interactions in between proteins, set out to establish a little protein particle that might bind to ACE2 much better than SARS-CoV-2 does however without impacting the receptor’s enzymatic activity.
The scientists, led byDr Ji ří Zahradn ík, a postdoctoral fellow in Schreiber’s group, started by determining SARS-CoV-2’s binding domain: the reasonably brief series of foundation within the bigger spike protein that physically binds to ACE2. Using the infection’s own receptor binding domain as a weapon versus it, Zahradn ík carried out a number of rounds of “evolution-in-a-test-tube,” established in Schreiber’s laboratory, on a genetically crafted pressure of baker’s yeast. Since yeast can be quickly controlled, Zahradn ík had the ability to quickly scan countless various anomalies that built up in the course of this synthetic advancement, a procedure that mimics natural advancement at a much faster rate. Ultimately, the objective was to discover a little particle that would be considerably “stickier” than the initial viral variation.
The fast evolutionary procedure led to a little protein piece with a binding ability 1,000 times more powerful than that of the initial viral binding domain
During this scanning procedure, Schreiber’s group provided strong proof in favor of the hypothesis that SARS-CoV-2 ends up being more infectious when anomalies enhance its fit to ACE2. The scientists discovered that currently after the preliminary of choice, the lab-made versions with tighter binding abilities to ACE2 simulated the anomalies present in the binding domains of the most infectious SARS-CoV-2 stress that had actually happened by methods of natural advancement, such as the British version (Alpha), the South African version (Beta) and the Brazilian version (Gamma). Surprisingly, the now prevalent Indian (Delta) alternative counts on a various technique to be more contagious– by partly averting detection by the body immune system.
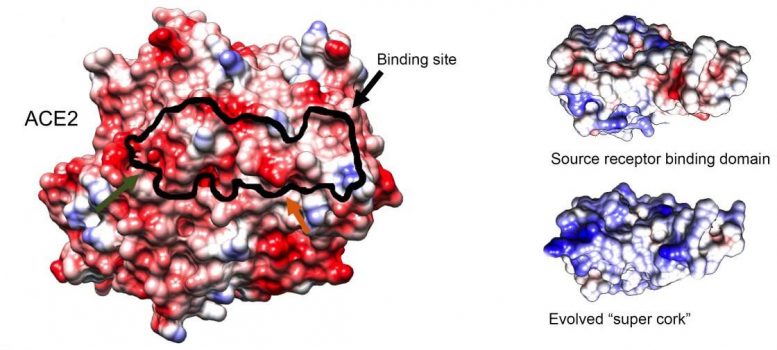
Structure of an ACE2 receptor (left), the initial binding particle (leading right) and the recently crafted “super cork” (bottom right), imaged by cryogenic electron microscopy carried out by Staff ScientistsDr Nadav Elad of Weizmann’s Chemical Research Support Department andDr Orly Dym of the Life Sciences Core FacilitiesDepartment The black overview shows the binding website of the “super cork” on the ACE2 receptor. Credit: Weizmann Institute of Science
Eventually, Zahradn ík separated a little protein piece with a binding ability 1,000 times more powerful than that of the initial binding domain from which it developed. This “super cork” not just healthy ACE2 like a glove, it was likewise discovered by Maya Shemesh and Shir Marciano, PhD trainees in Schreiber’s laboratory, to save the enzymatic activity of ACE2– simply as the scientists had actually planned. Furthermore, owing to the strong binding, extremely low concentrations of the recently crafted particle were required to accomplish the preferred stopping result.
While looking for a “super cork” that would obstruct the ACE2 receptor, the scientists taken a look at about 1,000,000,000 yeast mutants.
To establish a prospective approach for administering the particle as a drug, Schreiber and his group worked together withProf Yinon Rudich of Weizmann’s Earth and Planetary SciencesDepartment Together withDr Ira Marton andDr Chunlin Li, they developed an aerosol-based spray that would permit the industrialized particle to be supervised by inhalation to clients.
So far, the scientists have actually evaluated, at the NIH, the industrialized solution in hamsters contaminated with SARS-CoV-2. Preliminary results show that this treatment considerably decreases illness signs, recommending that it might be a prospective drug. More preclinical research studies are prepared to happen at the NIH in the future.
Reference: “SARS-CoV-2 variant prediction and antiviral drug design are enabled by RBD in vitro evolution” by Ji ří Zahradn ík, Shir Marciano, Maya Shemesh, Eyal Zoler, Daniel Harari, Jeanne Chiaravalli, Bj örn Meyer, Yinon Rudich, Chunlin Li, Ira Marton, Orly Dym, Nadav Elad, Mark G. Lewis, Hanne Andersen, Matthew Gagne, Robert A. Seder, Daniel C. Douek and Gideon Schreiber, 16 August 2021, Nature Microbiology
DOI: 10.1038/ s41564-021-00954 -4
Prof Gideon Schreiber’s research study is supported by the Ben B. and Joyce E. Eisenberg Foundation; the Rene and Tillie Molho Family Trust; Miel de Botton; and the Yotam Project.





