Severe COVID-19 triggers early lung capillary apoplexy, resulting in breathing distress, with research studies stressing timely anti-coagulation treatment to reduce problems.
Scientists from the University of São Paulo have actually found that extreme COVID-19 is mainly triggered by damage to the little capillary in the lungs, an outcome of SARS-CoV-2 infection.
Blood embolisms development (apoplexy) in the little capillary of the lungs is an early outcome of extreme < period class ="glossaryLink" aria-describedby ="tt" data-cmtooltip =(******************************************************************** )data-gt-translate-attributes="[{"attribute":"data-cmtooltip", "format":"html"}]" tabindex ="0" function ="link" > COVID-19, frequently happening before the breathing problems triggered by prevalent damage to the air sacs, according to aBrazilian research study reported in a short article released in theJournal ofAppliedPhysiologyPost- mortem assessments of 9 people who died from extreme COVID-19 exposed an unique pattern of modifications in lung capillary structure and apoplexy.(****************** )
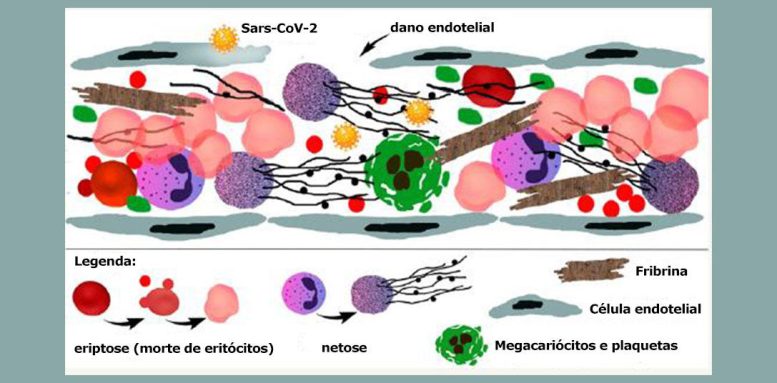
For the very first time, the post explains sub-cellular elements of the endothelial damage and associated thrombotic phenomena triggered by the infection.It keeps in mind the effect of intense swelling on lung microvascular flow as the essential consider extreme COVID -19, adding to a much deeper understanding of the pathophysiology of the illness and the advancement of unique healing methods.
“(*********************************************************************************************************************************** )research study provided the last evidence of what we had actually been mentioning because the really start of the pandemic– that extreme COVID-19 is a thrombotic illness.The< period class ="glossaryLink" aria-describedby ="tt" data-cmtooltip ="<div class=glossaryItemTitle>virus</div><div class=glossaryItemBody>A virus is a tiny infectious agent that is not considered a living organism. It consists of genetic material, either DNA or RNA, that is surrounded by a protein coat called a capsid. Some viruses also have an outer envelope made up of lipids that surrounds the capsid. Viruses can infect a wide range of organisms, including humans, animals, plants, and even bacteria. They rely on host cells to replicate and multiply, hijacking the cell's machinery to make copies of themselves. This process can cause damage to the host cell and lead to various diseases, ranging from mild to severe. Common viral infections include the flu, colds, HIV, and COVID-19. Vaccines and antiviral medications can help prevent and treat viral infections.</div>" data-gt-translate-attributes="[{"attribute":"data-cmtooltip", "format":"html"}]" tabindex ="0" function ="link" > infection< period class ="glossaryLink" aria-describedby ="tt" data-cmtooltip =(************************************************************************* )data-gt-translate-attributes="[{"attribute":"data-cmtooltip", "format":"html"}]" tabindex ="0" function ="link" > SARS-CoV-2 has a tropism for [is attracted to] the endothelium, the layer of cells that lines capillary.(************************************************************************************************************************* )it gets into endothelial cells, it initially impacts microvascular flow. The issue begins in the blood vessels of the lungs [the tiny blood vessels that surround the alveoli], followed by thickening in the bigger vessels that can reach any other organ,” stated pulmonologist Elnara Negri, very first author of the post and a teacher at the University of São Paulo’s Medical School (FM-USP). She was among the very first scientists worldwide to reach the conclusion that extreme COVID-19 is a thrombotic illness.
The scientists at USP examined lung tissue from 9 clients who passed away from COVID-19 Credit: Elia Caldini
In the research study, which was supported by FAPESP, the scientists utilized transmission and scanning electron microscopy to observe the results of the infection on lung endothelial cells from extreme COVID-19 clients who passed away at Hospital das Cl ínicas, the health center complex run by FM-USP.
All 9 samples acquired by minimally intrusive autopsies showed a high frequency of thrombotic microangiopathy– tiny embolism in little arteries and blood vessels that can result in organ damage and ischemic tissue injury. The samples originated from clients who were hospitalized in between March and May 2020, needed intubation and extensive care, and passed away owing to refractory hypoxemia and intense breathing failure.
It deserves keeping in mind that none of the clients consisted of in the research study was treated with anti-coagulants, as this was not part of the COVID-19 treatment procedure at the time. Nor were any COVID-19 vaccines readily available in the duration.
Endothelial glycocalyx shedding
Negri discussed that the endothelium is itself lined by a gel-like layer of glycoproteins called the glycocalyx, which serves as a barrier to control the gain access to of macromolecules and blood cells to the endothelial surface area. This barrier avoids thickening in capillary by hindering platelet interaction with the endothelium.
“Previous research studies carried out by Helena Nader at UNIFESP [the Federal University of São Paulo] revealed that SARS-CoV-2 gets into cells generally by binding to the receptor ACE-2 [a protein on the surface of various cell types, including epithelial and endothelial cells in the respiratory system] however before that, it binds to heparan sulfate [a polysaccharide], a significant element of the glycocalyx in endothelial cells. When it gets into the endothelium, it sets off shedding and damage of the glycocalyx, leading to tissue direct exposure and intravascular clotting. The procedure begins in the microcirculation,” Negri discussed.
Because the infection at first acts upon the lung microcirculation, contrast assessments carried out throughout the pandemic to examine the existence of embolism in bigger vessels in extreme COVID-19 clients stopped working to identify the issue at any early phase, she included. However, endothelial dysfunction is a crucial phenomenon in COVID-19 because it is straight connected with the activation of the inflammatory reaction that is particular of the illness.
“Massive viral invasion and destruction of the endothelium break down the endothelial barrier and impair the recruitment of circulating immune cells, activating pathways associated with thrombogenesis and inflammation,” she stated.
In the research study, the scientists discovered that endothelial injury tended to precede 2 typical procedures in cases of breathing distress: substantial alveolar-capillary membrane leak, and intra-alveolar build-up of fibrin (connected with blood clot and injury recovery).
A research study by the exact same group at FM-USP, led by Thais Mauad and consisting of transcriptomics (analysis of all < period class ="glossaryLink" aria-describedby ="tt" data-cmtooltip ="<div class=glossaryItemTitle>RNA</div><div class=glossaryItemBody>Ribonucleic acid (RNA) is a polymeric molecule similar to DNA that is essential in various biological roles in coding, decoding, regulation and expression of genes. Both are nucleic acids, but unlike DNA, RNA is single-stranded. An RNA strand has a backbone made of alternating sugar (ribose) and phosphate groups. Attached to each sugar is one of four bases—adenine (A), uracil (U), cytosine (C), or guanine (G). Different types of RNA exist in the cell: messenger RNA (mRNA), ribosomal RNA (rRNA), and transfer RNA (tRNA).</div>" data-gt-translate-attributes= "[{"attribute":"data-cmtooltip", "format":"html"}]" tabindex ="0" function ="link" > RNA records, coding, and non-coding), revealed that a number of paths connected with blood clot and platelet activation had actually been triggered prior to swelling in the lungs of clients with alveolar damage.
The analysis likewise validated that the clotting was not common of the normal procedure activated by the activation of coagulation aspects.”In COVID-19, the clotting is because of endothelial injury and intensified by NETosis[an immune mechanism involving programmed cell death via formation of neutrophil extracellular traps or NETs], dysmorphic red cell and platelet activation, all of that makes the blood thicker and triggers lots of problems,”Negri stated.
(********************** )When the blood is thick and extremely thrombogenic, she included, the client should be kept hydrated, whereas scattered alveolar damage in intense breathing distress syndromes due to other causes needs minimized hydration.“Also, the timing and rigorous control of anti-coagulation are fundamental,” she worried.
Another research study by the exact same group of scientists, consisting ofMarisaDolhnikoff andEliaCaldini, revealed lung damage in extreme COVID-19 to be connected with the degree of NETosis: the greater the level of Internet in lung tissue acquired by autopsy, the more the lungs were harmed.
Negri stated she started to presume there was a link in between COVID-19 and apoplexy early in the pandemic when she saw a phenomenon remembering her experience some 30 years ago with clients who had microvascular clotting after open-heart surgical treatment with extracorporeal flow and a bubble oxygenator, no longer utilized since it triggers endothelial damage.
“It was a widely used technique 30 years ago, but it causes lung injury very similar to that seen in COVID-19. So I’d already seen it. Besides the pulmonary injury, another similarity is the occurrence of peripheral thrombotic phenomena, such as red toes, for example,” she stated.
“As extreme COVID-19 embeds in, the drop in blood oxygen levels is secondary to lung capillary apoplexy. Initially, there’s no accumulation of fluid in the lungs, which aren’t ‘saturated’ and do not lose their compliance or flexibility. This implies the lungs in early extreme COVID-19 clients do not appear like sponges filled with liquid, as they carry out in intense breathing distress syndrome [ARDS] clients. On the contrary, the breathing failure connected with extreme COVID-19 includes dehydration of the lungs. The alveoli fill with air however the oxygen can’t go into the blood stream since of capillary clotting. This results in what we call ‘happy hypoxia’, where clients do not experience shortness of breath and aren’t conscious their oxygen saturation is precariously low.”
While observing the intubation of a serious COVID-19 client, Negri recognized the treatment of such cases need to be totally various from what it was at the start of the pandemic. “The secret to treating severe COVID-19 patients is keeping them hydrated and using anti-coagulant at the right dose, meaning the dose required in the hospital environment at the onset of oxygen desaturation, i.e. low levels of oxygen in the blood,” she stated. “After that, the therapeutic dose of anti-coagulant must be calculated daily on the basis of blood work, always in the hospital environment to avoid any risk of bleeding. Prophylaxis is required for an average of four to six weeks after discharge because that’s how long the endothelium takes to regenerate.”
This hydration and anti-coagulation procedure is required because, on the other hand with other type of ARDS in which oxygen in the lungs is avoided from going into the blood stream generally by alveolar swelling, lung capillary endothelial damage is the primary barrier in early extreme COVID-19, she discussed.
“No one learnt about this distinction in between COVID-19 and other kinds of ARDS at the really start of the pandemic. Indeed, this is why a lot of Italian clients passed away in ICUs [intensive care units], for instance. The treatment procedure utilized then was various,” she remembered.
In 2020, before the research study was reported in the Journal of Applied Physiology, Negri and her group had actually currently observed that making use of the anti-coagulant heparin enhanced oxygen saturation in crucial clients. In 2021, in cooperation with coworkers in a number of nations, they carried out a randomized scientific trial in which they prospered in showing that treatment with heparin minimized extreme COVID-19 death. The findings were released in the British Medical Journal
“That study helped bring about a global change in COVID-19 treatment guidelines by showing that COVID-19 mortality risk fell 78% when anti-coagulation was started in patients who needed oxygen supplementation but weren’t yet in intensive care,” Negri stated.
Endothelial dysfunction need to be reversed without hold-up in extreme COVID-19, utilizing an anti-coagulant, she discussed. “Blood clotting has to be stopped as soon as possible in order to avert the development of acute respiratory distress and other consequences of the disease, such as the problems now known as long COVID,” she stated.
An post just recently released in Nature Medicine by scientists connected with organizations in the United Kingdom strengthens the thrombotic nature of the illness, reporting a research study in which the just long COVID prognostic markers recognized were fibrinogen and D-dimer, proteins connected with coagulation.
“The study shows that long COVID results from inadequately treated thrombosis. The microcirculatory problem can persist in several organs, including the brain, heart, and muscles, as if the patient were having small heart attacks,” Negri stated.
Reference: “Ultrastructural characterization of alveolar microvascular damage in severe COVID-19 respiratory failure” by Elnara Marcia Negri, Marlene Benchimol, Thais Mauad, Amaro Nunes Duarte-Neto, Maiara Gottardi, Luiz Fernando Ferraz da Silva, Paulo Hilario Nascimento Saldiva, Marisa Dolhnikoff, Wanderley de Souza and Elia Garcia Caldini, 1 October 2023, Journal of Applied Physiology
DOI: 10.1152/ japplphysiol.004242023
“Acute blood biomarker profiles predict cognitive deficits 6 and 12 months after COVID-19 hospitalization” by Maxime Taquet, Zuzanna Skorniewska, Adam Hampshire, James D. Chalmers, Ling-Pei Ho, Alex Horsley, Michael Marks, Krisnah Poinasamy, Betty Raman, Olivia C. Leavy, Matthew Richardson, Omer Elneima, Hamish J. C. McAuley, Aarti Shikotra, Amisha Singapuri, Marco Sereno, Ruth M. Saunders, Victoria C. Harris, Linzy Houchen-Wolloff, Neil J. Greening, Parisa Mansoori, Ewen M. Harrison, Annemarie B. Docherty, Nazir I. Lone, Jennifer Quint, Naveed Sattar, Christopher E. Brightling, Louise V. Wain, Rachael E. Evans, John R. Geddes, Paul J. Harrison and PHOSP-COVID Study Collaborative Group, 31 August 2023, Nature Medicine
DOI: 10.1038/ s41591-023-02525- y
The research study was moneyed by the São Paulo Research Foundation.