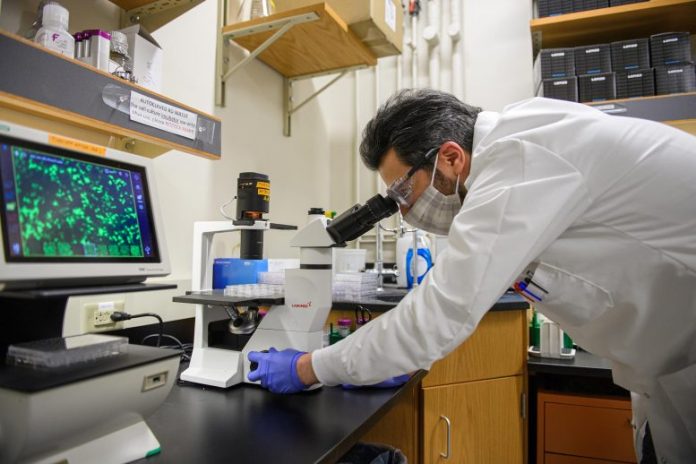
Scientists have actually found an unexpected action in lung cells contaminated with the SARS-CoV-2 infection, which may describe why the illness is so hard to deal with. “This was completely unexpected,” states Purdue researcher Majid Kazemian, who led the research study. The scientists recommend evaluating a brand-new pairing of drugs to fight the illness. Credit: Purdue University image/ Rebecca McElhoe
New insights into the immune action to SARS-CoV-2 infections might bring much better treatments for COVID-19 cases.
An global group of scientists all of a sudden discovered that a biochemical path, called the immune enhance system, is activated in lung cells by the infection, which may describe why the illness is so hard to deal with. The research study is released in the journal Science Immunology.
The scientists propose that the pairing of antiviral drugs with drugs that prevent this procedure might be more reliable. Using an in vitro design utilizing human lung cells, they discovered that the antiviral drug Remdesivir, in mix with the drug Ruxolitinib, hindered this enhance action.
This is in spite of current proof that trials of utilizing Ruxolitinib alone to deal with COVID-19 have actually not been assuring.
To recognize possible drug targets, Majid Kazemian, assistant teacher in the departments of computer technology and biochemistry at Purdue University, stated the research study group analyzed more than 1,600 formerly FDA-approved drugs with recognized targets.
“We looked at the genes that are up-regulated by COVID-19 but down-regulated by specific drugs, and Ruxolitinib was the top drug with that property,” he stated.
Within the last couple of years, researchers have actually found that the immune enhance system – an intricate system of little proteins produced by the liver that assists, or matches, the body’s antibodies in the battle versus blood-borne pathogens – can work within cells and not simply in the blood stream.
Surprisingly, the research study discovered that this action is activated in cells of the little structures in the lungs called alveoli, Kazemian stated.
“We observed that SARS-CoV2 infection of these lung cells causes expression of an activated complement system in an unprecedented way,” Kazemian stated. “This was completely unexpected to us because we were not thinking about activation of this system inside the cells, or at least not lung cells. We typically think of the complement source as the liver.”
Claudia Kemper, senior private investigator and chief of the Complement and Inflammation Research Section of the National Institutes of Health, was amongst the very first to identify unique functions of the enhance system in the body immune system. She concurred these newest findings are unexpected.
“The complement system is traditionally considered a liver-derived and blood-circulating sentinel system that protects the host against infections by bacteria, fungi and viruses,” she stated. “It is unexpected that in the setting of a SARS-CoV2 infection, this system rather turns against the host and contributes to the detrimental tissue inflammation observed in severe COVID-19. We need to think about modulation of this intracellular, local, complement when combating COVID-19.”
Dr. Ben Afzali, an Earl Stadtman Investigator of the National Institute of Health’s National Institute of Diabetes and Digestive and Kidney Diseases, stated there are now signs that this has ramifications for troubles in dealing with COVID-19.
“These findings provide important evidence showing not only that complement-related genes are amongst the most significant pathways induced by SARS-CoV2 in infected cells, but also that activation of complement occurs inside of lung epithelial cells, i.e., locally where infection is present,” he stated.
“This may explain why targeting the complement system outside of cells and in the circulation has, in general, been disappointing in COVID-19. We should probably consider using inhibitors of complement gene transcription or complement protein activation that are cell permeable and act intracellularly instead.”
Afzali warns that suitable medical trials must be carried out to develop whether a mix treatment supplies a survival advantage.
“The second finding that I think is important is that the data suggest potential benefit for patients with severe COVID-19 from combinatorial use of an antiviral agent together with an agent that broadly targets complement production or activation within infected cells,” he stated. “These data are promising, but it is important to acknowledge that we carried out the drug treatment experiments in cell lines infected with SARS-CoV2. So, in and of themselves they should not be used to direct treatment of patients.”
Kemper included that the unforeseen findings bring more concerns.
“A currently unexplored and possibly therapeutically interesting aspect of our observations is also whether the virus utilizes local complement generation and activation to its benefit, for example, for the processes underlying cell infection and replication,” she stated.
Reference: “SARS-CoV-2 drives JAK1/2-dependent local complement hyperactivation” by Bingyu Yan, Tilo Freiwald, Daniel Chauss, Luopin Wang, Erin West, Carmen Mirabelli, Charles J Zhang, Eva-Maria Nichols, Nazish Malik, Richard Gregory, Marcus Bantscheff, Sonja Ghidelli-Disse, Martin Kolev, Tristan Frum, Jason R Spence, Jonathan Z. Sexton, Konstantinos D. Alysandratos, Darrell N. Kotton, Stefania Pittaluga, Jack Bibby, Nathalie Niyonzima, Matthew R Olson, Shahram Kordasti, Didier Portilla, Christiane E Wobus, Arian Laurence, Michail S Lionakis, Claudia Kemper, Behdad Afzali and Majid Kazemian, 7 April 2021, Science Immunology.
DOI: 10.1126/sciimmunol.abg0833