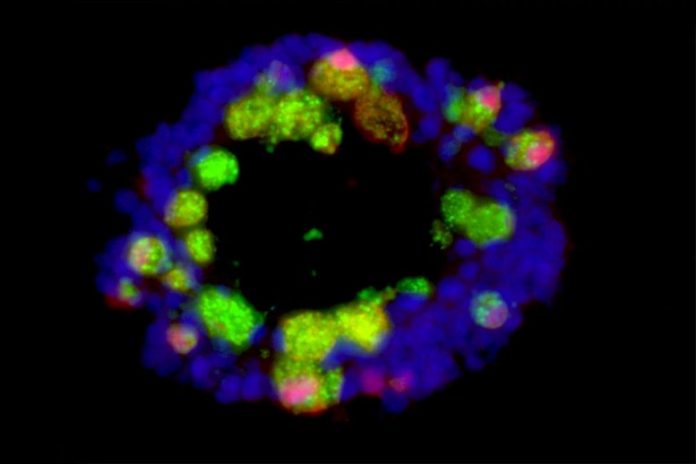
A small, 3D design of the intestinal tracts formed from anti-inflammatory cells referred to as Paneth cells (green and red) and other intestinal tract cells (blue) is seen in the image above. Researchers at Washington University School of Medicine in St. Louis and the Cleveland Clinic utilized such designs, called organoids, to comprehend why a Western-design diet plan abundant in fat and sugar damages Paneth cells and interrupts the gut body immune system. Credit: Ta-Chiang Liu
Diet abundant in sugar, fat damages immune cells in digestion systems of mice.
Eating a Western diet plan hinders the body immune system in the gut in manner ins which might increase danger of infection and inflammatory bowel illness, according to a research study from scientists at Washington University School of Medicine in St. Louis and Cleveland Clinic.
The research study, in mice and individuals, revealed that a diet plan high in sugar and fat causes damage to Paneth cells, immune cells in the gut that assist keep swelling in check. When Paneth cells aren’t operating appropriately, the gut body immune system is exceedingly susceptible to swelling, putting individuals at danger of inflammatory bowel illness and weakening efficient control of disease-causing microorganisms. The findings, released today (May 18, 2021) in Cell Host & Microbe, open brand-new methods to controling gut resistance by bring back typical Paneth cell function.
“Inflammatory bowel disease has historically been a problem primarily in Western countries such as the U.S., but it’s becoming more common globally as more and more people adopt Western lifestyles,” stated lead author Ta-Chiang Liu, MD, PhD, an associate teacher of pathology & immunology at Washington University. “Our research showed that long-term consumption of a Western-style diet high in fat and sugar impairs the function of immune cells in the gut in ways that could promote inflammatory bowel disease or increase the risk of intestinal infections.”
Paneth cell disability is an essential function of inflammatory bowel illness. For example, individuals with Crohn’s illness, a type of inflammatory bowel illness identified by stomach discomfort, diarrhea, anemia, and tiredness, typically have actually Paneth cells that have quit working.
Liu and senior author Thaddeus Stappenbeck, MD, PhD, chair of the Department of Inflammation and Immunity at Cleveland Clinic, set out to discover the reason for Paneth cell dysfunction in individuals. They examined a database consisting of market and scientific information on 400 individuals, consisting of an evaluation of everyone’s Paneth cells. The scientists discovered that high body mass index (BMI) was connected with Paneth cells that looked irregular and unhealthy under a microscopic lense. The greater an individual’s BMI, the even worse his/her Paneth cells looked. The association held for healthy grownups and individuals with Crohn’s illness.
To much better comprehend this connection, the scientists studied 2 pressures of mice that are genetically inclined to weight problems. Such mice chronically overindulge since they bring anomalies that avoid them from feeling complete even when fed a routine diet plan. To the scientists’ surprise, the overweight mice had Paneth cells that looked typical.
In individuals, weight problems is regularly the outcome of consuming a diet plan abundant in fat and sugar. So the researchers fed typical mice a diet plan in which 40% of the calories originated from fat or sugar, comparable to the normal Western diet plan. After 2 months on this chow, the mice had actually ended up being overweight and their Paneth cells looked distinctly irregular.
“Obesity wasn’t the problem per se,” Liu stated. “Eating too much of a healthy diet didn’t affect the Paneth cells. It was the high-fat, high-sugar diet that was the problem.”
The Paneth cells went back to typical when the mice were returned on a healthy mouse diet plan for 4 weeks. Whether individuals who repeatedly consume a Western diet plan can enhance their gut resistance by altering their diet plan stays to be seen, Liu stated.
“This was a short-term experiment, just eight weeks,” Liu stated. “In people, obesity doesn’t occur overnight or even in eight weeks. People have a suboptimal lifestyle for 20, 30 years before they become obese. It’s possible that if you have Western diet for so long, you cross a point of no return and your Paneth cells don’t recover even if you change your diet. We’d need to do more research before we can say whether this process is reversible in people.”
Further experiments revealed that a particle referred to as deoxycholic acid, a secondary bile acid formed as a by-product of the metabolic process of gut germs, forms the link in between a Western diet plan and Paneth cell dysfunction. The bile acid increases the activity of 2 immune particles — farnesoid X receptor and type 1 interferon — that hinder Paneth cell function.
Liu and coworkers now are examining whether fat or sugar plays the main function in impairing Paneth cells. They likewise have actually started studying methods to bring back typical Paneth cell function and enhance gut resistance by targeting the bile acid or the 2 immune particles.
Reference: 18 May 2021, Cell Host & Microbe.
DOI: 10.1016/j.chom.2021.04.004
Funding: National Institutes of Health, the Helmsley Charitable Trust, Washington University’s Genome Technology Access Center, Washington University’s Digestive Disease Research Core Center