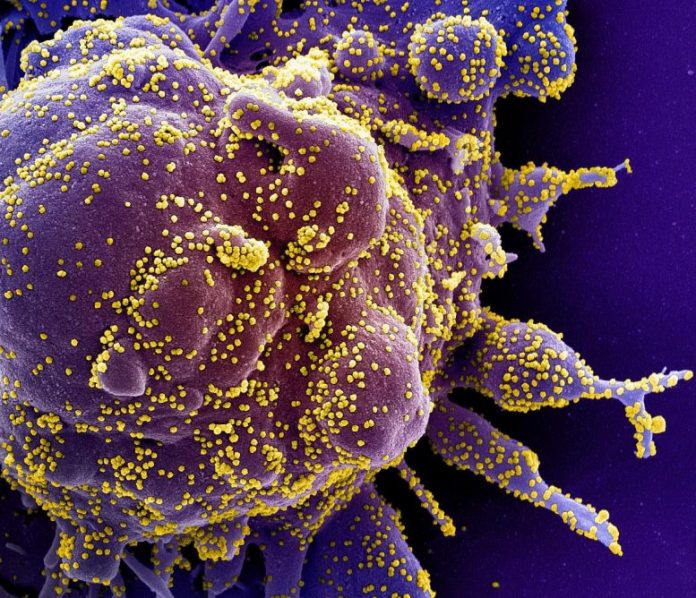
Colorized scanning electron micrograph of a cell (purple) greatly contaminated with SARS-CoV-2 infection particles (yellow). A current research study by Johns Hopkins Medicine reveals that obstructing a particular protein in a biological path might avoid SARS-CoV-2 infection and keep the infection from misdirecting the body immune system versus healthy cells and organs. Credit: National Institute of Allergy and Infectious Diseases, National Institutes of Health
Blocking Immune System Pathway May Stop COVID-19 Infection, Prevent Severe Organ Damage
While the world waits excitedly for a safe and reliable vaccine to avoid infections from extreme intense breathing syndrome coronavirus 2 (SARS-CoV-2), the infection behind the COVID-19 pandemic, scientists likewise are concentrating on much better understanding how SARS-CoV-2 assaults the body in the look for other methods of stopping its disastrous effect. The secret to one possibility — obstructing a protein that allows the infection to turn the body immune system versus healthy cells — has actually been determined in a current research study by a group of Johns Hopkins Medicine scientists.
Based on their findings, the scientists think that preventing the protein, referred to as aspect D, likewise will reduce the possibly fatal inflammatory responses that numerous clients need to the infection.
Making the discovery much more amazing is that there might currently be drugs in advancement and screening for other illness that can do the needed stopping.
The research study was released just recently in the journal Blood.
Scientists currently understand that spike proteins on the surface area of the SARS-CoV-2 infection — making the pathogen appear like the spiny ball from a middle ages mace — are the methods by which it connects to cells targeted for infection. To do this, the spikes initially clinch heparan sulfate, a big, intricate sugar particle discovered on the surface area of cells in the lungs, capillary and smooth muscle comprising most organs. Facilitated by its preliminary binding with heparan sulfate, SARS-CoV-2 then utilizes another cell-surface element, the protein referred to as angiotensin-converting enzyme 2 (ACE2), as its entrance into the assaulted cell.
The Johns Hopkins Medicine group found that when SARS-CoV-2 bind heparan sulfate, it avoids aspect H from utilizing the sugar particle to bind with cells. Factor H’s regular function is to manage the chemical signals that activate swelling and keep the body immune system from damaging healthy cells. Without this security, cells in the lungs, heart, kidneys and other organs can be ruined by the defense reaction nature planned to protect them.
“Previous research has suggested that along with tying up heparan sulfate, SARS-CoV-2 activates a cascading series of biological reactions — what we call the alternative pathway of complement, or APC — that can lead to inflammation and cell destruction if misdirected by the immune system at healthy organs,” states research study senior author Robert Brodsky, M.D., director of the hematology department at the Johns Hopkins University School of Medicine. “The goal of our study was to discover how the virus activates this pathway and to find a way to inhibit it before the damage happens.”
The APC is among 3 domino effect procedures including the splitting and integrating of more than 20 various proteins — referred to as enhance proteins — that typically gets triggered when germs or infections attack the body. The final product of this enhance waterfall, a structure called membrane attack complex (MAC), forms on the surface area of the intruder and triggers its damage, either by developing holes in bacterial membranes or interrupting an infection’ external envelope. However, MACs likewise can emerge on the membranes of healthy cells. Fortunately, human beings have a variety of enhance proteins, consisting of aspect H, that manage the APC, keep it in check and for that reason, safeguard regular cells from damage by MACs.
In a series of experiments, Brodsky and his associates utilized regular human blood serum and 3 subunits of the SARS-CoV-2 spike protein to find precisely how the infection triggers the APC, pirates the body immune system and threatens regular cells. They found that 2 of the subunits, called S1 and S2, are the parts that bind the infection to heparan sulfate — triggering the APC waterfall and obstructing aspect H from getting in touch with the sugar — and in turn, disabling the enhance policy by which aspect H prevents a misdirected immune reaction.
In turn, the scientists state, the resulting body immune system reaction to chemicals launched by the lysing of eliminated cells might be accountable for the organ damage and failures seen in extreme cases of COVID-19.
Most especially, Brodsky states, the research study group discovered by obstructing another enhance protein, referred to as aspect D, which works right away upstream in the path from aspect H, they had the ability to stop the devastating chain of occasions activated by SARS-CoV-2.
“When we added a small molecule that inhibits the function of factor D, the APC wasn’t activated by the virus spike proteins,” Brodsky states. “We believe that when the SARS-CoV-2 spike proteins bind to heparan sulfate, it triggers an increase in the complement-mediated killing of normal cells because factor H, a key regulator of the APC, can’t do its job.”
To much better comprehend what occurs, Brodsky states think about the APC like a cars and truck in movement.
“If the brakes are disabled, the gas pedal can be floored without restraint, very likely leading to a crash and destruction,” he describes. “The viral spike proteins disable the biological brakes, factor H, enabling the gas pedal, factor D, to accelerate the immune system and cause cell, tissue and organ devastation. Inhibit factor D, and the brakes can be reapplied and the immune system reset.”
Brodsky includes that cell death and organ damage from a misdirected APC related to aspect H suppression is currently understood to happen in numerous complement-related human illness, consisting of age-related macular degeneration, a leading reason for vision loss for individuals age 50 and older; and irregular hemolytic uremic syndrome (aHUS), an unusual illness that triggers embolisms to obstruct blood circulation to the kidneys.
Brodsky and his associates hope that their work will motivate more research study into the possible usage versus COVID-19 of complement-inhibiting drugs currently in the pipeline for other illness.
“There are a number of these drugs that will be FDA-approved and in clinical practice within the next two years,” Brodsky states. “Perhaps one or more of these could be teamed with vaccines to help control the spread of COVID-19 and avoid future viral pandemics.”
Reference: “Direct activation of the alternative complement pathway by SARS-CoV-2 spike proteins is blocked by factor D inhibition” by Jia Yu, Xuan Yuan, Hang Chen, Shruti Chaturvedi, Evan M. Braunstein and Robert A. Brodsky, 2 September 2020, Blood.
DOI: 10.1182/blood.2020008248
Along with Brodsky, the other members of the Johns Hopkins Medicine research study group are lead author Jia Yu; Xuan Yuan; Hang Chen; Shruti Chaturvedi, M.B.B.S.; and Evan Braunstein, M.D., Ph.D.
The research study was supported by National Heart, Lung and Blood Institute grant R01 HL133113.
Disclaimer: Johns Hopkins Medicine scientists are working relentlessly to discover methods to much better comprehend and ultimately remove COVID-19 and the infection that triggers it. Discoveries like this one, particularly those associated to scientific treatments and drug programs, are still early in principle and little in sample size. This will need extensive research study, screening and peer evaluation, all of which take some time, prior to strong conclusions for scientific care and illness avoidance can be made.