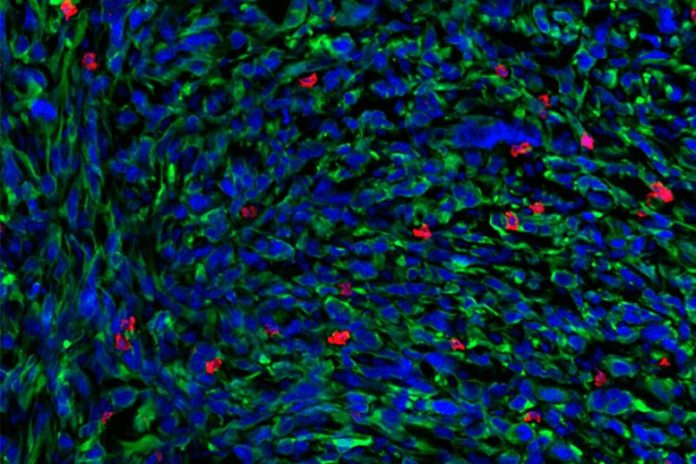
The scientists took this picture of a growth utilizing immunofluorescence, a strategy that enables them to stain tissue areas with fluorescently-labeled antibodies or dyes. Blue shows the cell nuclei, green represents growth areas, and red is a marker for T cells. Credit: Elen Torres-Mejia
Researchers analyze when and why immune cells stop working to react to immunotherapy, recommending that T cells require a various type of prodding to re-engage the immune reaction.
Non- little cell lung cancer (NSCLC) is the most typical kind of lung cancer in human beings. Some clients with NSCLC get a treatment called immune checkpoint blockade (ICB) that assists eliminate cancer cells by revitalizing a subset of immune cells called T cells, which are “exhausted” and have actually quit working. However, just about 35% of NSCLC clients react to ICB treatment. Stefani Spranger’s laboratory at the MIT Department of Biology checks out the systems behind this resistance, with the objective of motivating brand-new treatments to much better deal with NSCLC clients. In a brand-new research study released onOct 29 in Science Immunology, a group led by Spranger laboratory postdoc Brendan Horton exposed what triggers T cells to be non-responsive to ICB– and recommends a possible option.
Scientists have actually long believed that the conditions within a growth was accountable for identifying when T cells quit working and end up being tired after being overstimulated or working for too long to combat a growth. That’s why doctors recommend ICB to deal with cancer– ICB can rejuvenate the tired T cells within a growth. However, Horton’s brand-new experiments reveal that some ICB-resistant T cells quit working prior to they even go into the growth. These T cells are not really tired, however rather they end up being inefficient due to modifications in gene expression that develop early throughout the activation of a T cell, which happens in lymph nodes. Once triggered, T cells separate into particular practical states, which are appreciable by their distinct gene expression patterns.
The idea that the inefficient state that causes ICB resistance emerges prior to T cells go into the growth is rather unique, states Spranger, the Howard S. and Linda B. Stern Career Development Professor, a member of the Koch Institute for Integrative Cancer Research, and the research study’s senior author.
“We show that this state is actually a preset condition, and that the T cells are already non-responsive to therapy before they enter the tumor,” she states. As an outcome, she describes, ICB treatments that work by revitalizing tired T cells within the growth are less most likely to be efficient. This recommends that integrating ICB with other types of immunotherapy that target T cells in a different way may be a more efficient method to assist the body immune system fight this subset of lung cancer.
In order to identify why some growths are resistant to ICB, Horton and the research study group studied T cells in murine designs of NSCLC. The scientists sequenced messenger RNA from the responsive and non-responsive T cells in order to recognize any distinctions in between the T cells. Supported in part by the Koch Institute Frontier Research Program, they utilized a strategy called Seq-Well, established in the laboratory of fellow Koch Institute member J. Christopher Love, the Raymond A. (1921) and Helen E.St Laurent Professor of Chemical Engineering and a co-author of the research study. The method enables the fast gene expression profiling of single cells, which allowed Spranger and Horton to get an extremely granular take a look at the gene expression patterns of the T cells they were studying.
Seq-Well exposed unique patterns of gene expression in between the responsive and non-responsive T cells. These distinctions, which are identified when the T cells presume their specialized practical states, might be the underlying reason for ICB resistance.
Now that Horton and his associates had a possible description for why some T cells did not react to ICB, they chose to see if they might assist the ICB-resistant T cells eliminate the growth cells. When evaluating the gene expression patterns of the non-responsive T cells, the scientists had actually observed that these T cells had a lower expression of receptors for particular cytokines, little proteins that manage body immune system activity. To combat this, the scientists dealt with lung growths in murine designs with additional cytokines. As an outcome, the formerly non-responsive T cells were then able to combat the growths– indicating that the cytokine treatment avoided, and possibly even reversed, the dysfunctionality.
Administering cytokine treatment to human clients is not presently safe, due to the fact that cytokines can trigger severe negative effects in addition to a response called a “cytokine storm,” which can produce serious fevers, swelling, tiredness, and queasiness. However, there are continuous efforts to find out how to securely administer cytokines to particular growths. In the future, Spranger and Horton think that cytokine treatment might be utilized in mix with ICB.
“This is potentially something that could be translated into a therapeutic that could increase the therapy response rate in non-small cell lung cancer,” Horton states.
Spranger concurs that this work will assist scientists establish more ingenious cancer treatments, specifically due to the fact that scientists have actually traditionally concentrated on T cell fatigue instead of the earlier function that T cell practical states may play in cancer.
“If T cells are rendered dysfunctional early on, ICB is not going to be effective, and we need to think outside the box,” she states. “There’s more evidence, and other labs are now showing this as well, that the functional state of the T cell actually matters quite substantially in cancer therapies.” To Spranger, this suggests that cytokine treatment “might be a therapeutic avenue” for NSCLC clients beyond ICB.
Jeffrey Bluestone, the A.W. and Mary Margaret Clausen Distinguished Professor of Metabolism and Endocrinology at the University of California-San Francisco, who was not included with the paper, concurs. “The study provides a potential opportunity to ‘rescue’ immunity in the NSCLC non-responder patients with appropriate combination therapies,” he states.
This research study was moneyed by the Pew-Stewart Scholars for Cancer Research, the Ludwig Center for Molecular Oncology, the Koch Institute Frontier Research Program through the Kathy and Curt Mable Cancer Research Fund, and the National Cancer Institute.