Researchers at the Icahn School of Medicine at Mount Sinai discovered that the majority of disease-causing anomalies have a low danger of in fact triggering illness. Credit: Courtesy of Do laboratory, Mount Sinai, N.Y., N.Y.
Results of big biobank research study by Mount Sinai scientists might assist physicians much better examine real illness danger.
Imagine getting a favorable outcome on a hereditary test. The medical professional informs you that you have a “pathogenic genetic variant,” or a DNA series that is understood to raise the possibilities for getting an illness like breast cancer or diabetes. But exactly what are those possibilities– 10 percent? Fifty percent? One hundred? Currently, that is not a simple concern to respond to.
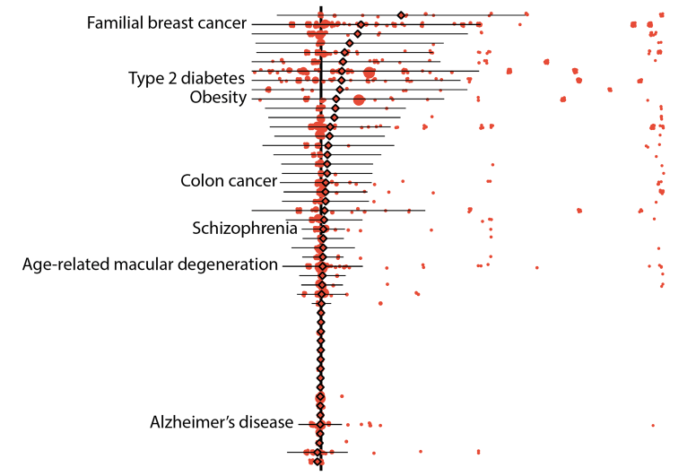
To address this requirement, scientists at the Icahn School of Medicine at Mount Sinai evaluated the DNA series and electronic health record information of countless people saved in 2 huge biobanks. Overall, they found that the possibility a pathogenic hereditary version might in fact trigger an illness is fairly low– about 7 percent. Nonetheless, they likewise discovered that some variations, such as those related to breast cancer, are connected to a wide variety of threats for illness. The results, released in JAMA, might change the method the threats related to these variations are reported, and one day, aid assist the method doctors analyze hereditary screening outcomes.
“A major goal of this study was to produce helpful, advanced statistics which quantitatively assess the impact that known disease-causing genetic variants may have on an individual’s risk to disease,” stated Ron Do, PhD, Associate Professor of Genetics and Genomic Sciences and a member of The Charles Bronfman Institute for Personalized Medicine at Icahn Mount Sinai.
Over the past 20 years researchers have actually found numerous countless variations that might trigger a range of illness. However, due to the nature of these discoveries, it has actually been challenging to approximate– or offer data on– the real danger of this taking place for each gene version. So far, the majority of price quotes have actually been based upon research studies including a little number of topics, who were either part of a household that had a history of having an illness or were hired at disease-specific centers. But research studies like these that do not utilize arbitrarily picked big populations might produce overestimates of the danger postured by variations.
In this research study, the scientists dealt with the concern by browsing massive DNA sequencing information of 72,434 people for 37,780 recognized variations and after that scanning each person’s health records for a matching illness medical diagnosis. The substantial search included 29,039 individuals in Mount Sinai’s BioMe ® Biobank program and 43,395 individuals who became part of the UK Biobank.
The research study was led by Iain S. Forrest, an MD-PhD prospect inDr Do’s laboratory who discovered motivation from previous scientific experience he had as part of a postbaccalaureate fellowship at the National Institutes of Health (NIH).
“The idea for the study came out of a brainstorming session,” statedMr Forrest. “Dr. Do and I discussed the need to have a better system for classifying disease risk. Currently, variants are categorized by broad labels such as ‘pathogenic’ or ‘benign.’ As I learned in the clinic, there’s a lot of grey area with these labels. That’s when we realized that the biobanks which link DNA sequence data to electronic health records are an unparalleled opportunity to address this need.”
Initial results revealed that 157 illness in their information set might be connected to 5,360 variations that were specified as either “pathogenic” by ClinVar, a commonly referenced, NIH-supported town library, or “loss-of-function” as forecasted by bioinformatic algorithms. On average, the “penetrance,” or possibility that a variation was connected to an illness medical diagnosis, was low, particularly 6.9 percent. Likewise, the typical danger distinction, which explains the boost in illness danger for a person who has the version over a person who does not have it, was likewise low.
“At first I was quite surprised by the results. The risks we discovered were lower than I expected,” statedDr Do. “These results raise questions about how we should be classifying the risks of these variants.”
Despite these outcomes, the threats related to some hereditary variations stayed high. For circumstances, pathogenic variations of the breast cancer genes BRCA1 and BRCA2 both balanced 38 percent penetrance, with specific variations falling in between no and 100 percent.
Further results shown other benefits of utilizing biobank information. In one example, the scientists had the ability to compute the threats of specific variations that are related to age-related conditions, such as some types of type 2 diabetes and breast and prostate cancers. On average, the penetrance of these variations had to do with 10 percent for people over 70 years of age whereas it had to do with 8 percent for those who were older than 20.
The group likewise discovered that the existence of some variations might depend upon a person’s ethnic culture and recognized more than 100 variations that are particularly discovered in people of non-European descent.
Finally, the authors noted numerous possible methods the research study itself might have under- or overstated the threats reported.
“While more research is needed to be done, we feel that this study is a good first step towards eventually providing doctors and patients with the accurate and nuanced information they need to make more precise diagnoses,” statedDr Do.
Reference: “Population-Based Penetrance of Deleterious Clinical Variants” by Iain S. Forrest, BS; Kumardeep Chaudhary, PhD; Ha My T. Vy, PhD; Ben O. Petrazzini, BS; Shantanu Bafna, MS; Daniel M. Jordan, PhD; Ghislain Rocheleau, PhD; Ruth J. F. Loos, PhD; Girish N. Nadkarni, MD; Judy H. Cho, MD and Ron Do, PhD, 25 January 2022,
DOI: 10.1001/ jama.202123686
This work was supported by the National Institutes of Health (GM124836, GM007280, HL139865, and HL155915).