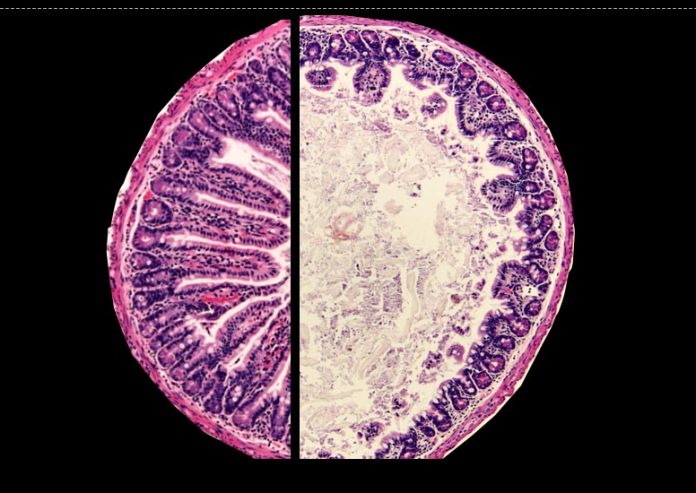
Healthy mouse intestinal tract with long, finger-like villi (left) and intestinal tract of mouse with ecological enteric dysfunction with reduced villi (right). Credit: Amrita Bhattacharjee
A persistent gut condition that takes place in areas with bad sanitation interrupts digestive immune reactions and hinders oral vaccine efficiency in a mouse design of the illness, according to research study led by UPMC Children’s Hospital of Pittsburgh and University of Pittsburgh School of Medicine researchers.
The finding, released today (August 3, 2021) in Immunity, is very important due to the fact that oral vaccines provided by liquid drops to the mouth, such as polio and rotavirus vaccines, are particularly helpful in low-income nations that might not have healthcare employees trained in administering vaccines through needles. They might likewise promote much better regional resistance in the gut, which is crucial for warding off illness contracted by infected food and water — consisting of a few of the really infections that add to the gut condition, called ecological enteric dysfunction, or EED.
“It is tragic that the exact vaccines that might help prevent EED don’t work in children who have the disease,” stated Timothy Hand, Ph.D., senior author of the research study and assistant teacher of pediatrics and immunology at the R.K. Mellon Institute for Pediatric Research at UPMC Children’s and director of Pitt’s Gnotobiotic Core.
EED is brought on by poor nutrition and persistent intestinal infection from infected food and water. Infection with infections, parasites or germs integrated with bad diet plan can set off gut swelling and damage the finger-like forecasts called villi that assist take in nutrients from food.
“EED can affect anyone, but it’s a major problem in children because they’re still developing,” stated Hand. “The result is that children with EED are stunted. They end up shorter in stature. But perhaps more importantly, it can significantly affect brain development: These children have less cognitive ability. And this is a lifelong problem; you can’t restore that development later in life.”
To find out more about the systems behind oral vaccine failure, Hand and his group established a mouse design of the illness. They caused EED-like signs by feeding the rodents a diet plan lacking in fat and protein and inoculating them with a pressure of E. coli germs that attacks gut cells.
Like human beings with the illness, EED mice had actually stunted development, shifts in the gut microbiome structure, raised gut swelling and reduced gut villi compared to control mice that got a typical diet plan with sufficient fat and protein or animals that got a typical diet plan and germs or a bad diet plan without germs.
After offering the mice an oral vaccine, the scientists discovered that immune reactions were seriously jeopardized in those with EED. Vaccine-particular CD4+ T cells in the little intestinal tract had to do with 18 times lower than in control mice.
Further experiments showed that oral vaccine failure in EED mice was moderated by their gut microbiome. In reaction to microbiome-associated swelling, T regulative (Treg) cells collect in the little intestinal tract of EED mice.
“Treg cells arise because there’s too much inflammation and they help tamp down that inflammation,” stated Hand. “But unfortunately, a side effect is that they prevent local accumulation of vaccine-specific CD4+ T cells.”
When the group utilized prescription antibiotics to remove gut germs, vaccine efficiency was brought back in EED mice.
According to Hand, these findings support the concept that targeting the microbiome might assist deal with EED and enhance vaccine success in kids.
“Judicious use of antibiotics in these children might be able to reset the small intestinal microbiome, reduce inflammation in the small intestine and reduce those Tregs,” he stated.
EED is uncommon in resource-rich nations however typical in poorer nations that do not have sewer system and sanitation. About 150 million kids around the world reside in conditions that put them at threat of getting the illness.
“If we could get flush toilets and plumbing to the world, we wouldn’t have this disease,” stated Hand. “What’s causing these chronic infections is that people are either drinking contaminated water or flies are transporting diseases from sewage to food.”
In the future, Hand and his group strategy to work together with scientists in nations where EED is an issue to much better comprehend vaccine results in kids with this illness.
Reference: “Environmental enteric dysfunction induces regulatory T cells that inhibit local CD4+ T cell responses and impair oral vaccine efficacy” by Amrita Bhattacharjee, Ansen H.P. Burr, Abigail E. Overacre-Delgoffe, Justin T. Tometich, Deyi Yang, Brydie R. Huckestein, Jonathan L. Linehan, Sean P. Spencer, Jason A. Hall, Oliver J. Harrison, Denise Morais da Fonseca, Elizabeth B. Norton, Yasmine Belkaid and Timothy W. Hand, 3 August 2021, Immunity.
DOI: 10.1016/j.immuni.2021.07.005
Additional authors on the research study are Amrita Bhattacharjee, Ph.D., Ansen H.P. Burr, Abigail E. Overacre-Delgoffe, Ph.D., Justin T. Tometich and Brydie R. Huckestein, all of Pitt or UPMC, or both; Deyi Yang, of UPMC and Central South University, China; Jonathan L. Linehan, Ph.D., Sean P. Spencer, M.D., Ph.D., Jason A. Hall, Ph.D., Oliver J. Harrison, Ph.D., Denise Morais da Fonseca, Ph.D., and Yasmine Belkaid, PhD., all of the National Institutes of Health; and Elizabeth B. Norton, Ph.D., of Tulane University.
This research study was supported by National Institutes of Health awards R21AI142051, 2015/25364-0 and T32AI089443, the R.K. Mellon Institute for Pediatric Research and UPMC Children’s Hospital of Pittsburgh.